Modern healthcare is fragmented. Understanding helps connect the dots.
Modern healthcare is fragmented. Understanding helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
Post Concussion Syndrome Treatment: A Practical Guide to Recovery
January 21, 2026 13 min read
Living with symptoms long after a head injury can be confusing and frustrating. If you are searching for clear information on post concussion syndrome treatment, you have likely found conflicting advice and promises that don't seem to match your experience.
Many people are told their condition is difficult to treat, which only adds to the uncertainty. This article is designed to offer clarity, not miracle claims.
We will explain how healthcare professionals approach this condition. The focus is not on quick fixes, but on understanding the underlying issues, which allows for a more effective, active approach to recovery.
Why Concussion Symptoms Can Persist
When symptoms like headaches, brain fog, and fatigue continue for weeks or months after an injury, it is often diagnosed as post concussion syndrome (PCS). This is a recognised clinical condition, not a sign that you aren't trying hard enough to get better.
The persistence of these symptoms is often misunderstood. It is not typically due to ongoing structural brain damage, but rather a disruption in how the brain regulates its energy and communicates with other body systems.

The Brain's Energy Deficit
After a concussion, the communication link between brain cells and the blood vessels that supply them with fuel (oxygen and glucose) can become inefficient. In clinical settings, this is sometimes referred to as neurovascular coupling dysfunction.
This means your brain has to work significantly harder to perform routine tasks. This increased effort drains your "mental battery" much faster than usual, leading to common PCS symptoms:
- Headaches or migraines
- Persistent brain fog
- Dizziness or a feeling of imbalance
- Overwhelming fatigue
This state of high effort and low energy helps explain why activities that were once simple, like reading an email or visiting a supermarket, can now feel exhausting and trigger a flare-up of symptoms.
Understanding the "Boom-and-Bust" Cycle
Symptoms often linger because of this ongoing energy deficit. When you push past your new, lower energy limit, your brain cannot cope, and your symptoms intensify.
This creates a frustrating cycle of "good days" and "bad days," making it difficult to plan your life.
This pattern is not a personal failing; it is an important clinical sign. It indicates that the brain’s regulatory systems are out of sync and require targeted rehabilitation to recalibrate. Modern post concussion syndrome treatment is designed to provide this support.
Our goal is to replace uncertainty with understanding. By explaining the mechanisms behind your symptoms, we can establish a solid foundation for effective recovery strategies. For a closer look at the studies informing these concepts, you can review our list of concussion-related references.
Core Principles of Active Rehabilitation
Effective management of post-concussion syndrome is an active process. It is not about passively waiting for time to heal the injury. Modern treatment focuses on active rehabilitation, guided by two core principles.
For many years, the standard advice was prolonged rest, sometimes called ‘cocoon therapy’. We now understand that for many people with persistent symptoms, this approach may be counterproductive. The focus has shifted to helping you work with your brain's healing process.

Respecting the Brain's Energy Limits
First, it is essential to acknowledge that the brain is experiencing a temporary but real energy deficit.
Imagine your brain’s energy as a phone battery. Before the injury, it likely held a full charge all day. After a concussion, that same battery might drain quickly after minimal mental or physical effort. This is a physiological change, not a lack of willpower.
Attempting to 'push through' symptoms like a headache or brain fog forces an already strained system to work harder. This often worsens the energy debt, leading to a significant symptom flare-up and a period of forced rest. The first principle is learning to manage this limited energy supply.
Finding Your Sub-Symptom Threshold
The second principle is sub-symptom threshold activity. This involves finding a level of activity that gently stimulates the brain and body without making symptoms significantly worse.
Think of it as carefully watering a plant. Too little, and it won't grow; too much, and it will be overwhelmed. You are looking for the right amount of activity that encourages healing without causing a setback.
This approach changes your relationship with your symptoms. They are no longer an enemy to be defeated. Instead, they become useful feedback—a signal to ease off, not a sign of failure.
Your threshold will likely change from day to day. This is normal. The goal is to listen to your body and gradually expand that threshold over time.
This active, gradual approach is supported by current research. For example, one major study found that 45% of patients still had symptoms six months post-injury, challenging the older notion that most people recover without intervention. A lack of clear, active protocols can contribute to these prolonged recoveries. You can read more about post-concussion syndrome recovery patterns in the UK to see the data.
By adopting these two principles, you become an active participant in your healing. For readers who want a more structured overview of this process, our collection of patient guides for head-related conditions offers a clear, organised framework.
Key Therapies for Post-Concussion Syndrome
Treating post-concussion syndrome effectively involves actively retraining the specific brain and body systems affected by the injury.
This is similar to recovering from a joint injury. You would work with a physiotherapist to strengthen supporting muscles and restore proper movement. PCS recovery follows a similar logic, using targeted therapies to address the root cause of symptoms.
Clinicians use several evidence-based therapies to help the brain recalibrate. The goal is not to push through pain, but to provide gentle, consistent signals that encourage the brain to function more efficiently.
Vestibular Therapy for Dizziness and Balance
A persistent feeling of dizziness, vertigo, or being off-balance is a common symptom of PCS. This often occurs because the concussion has disrupted signals from your vestibular system—the part of your inner ear responsible for balance and spatial orientation.
Vestibular therapy is a specialised form of physiotherapy designed to improve communication between the brain and the inner ear. A trained therapist guides you through specific exercises, which may include:
- Gaze stabilisation exercises: Focusing on a fixed point while moving your head.
- Balance training: Using different surfaces or postures to improve stability.
- Habituation exercises: Gently and repeatedly exposing you to movements that trigger dizziness to help your brain adapt and become less sensitive.
The goal is to retrain the brain to trust the signals it receives from the vestibular system, which can significantly reduce dizziness.
Vision Therapy for Headaches and Sensory Overload
Many people with PCS experience eye fatigue, difficulty focusing, or feeling overwhelmed by bright lights and busy environments. These visual problems are a major trigger for headaches and cognitive fatigue.
This occurs because the injury can disrupt the coordination between your eyes and your brain. Vision therapy, often overseen by a neuro-optometrist, addresses these specific issues. It is more than a standard eye test; it is like physiotherapy for your visual system.
Therapy may involve exercises to improve:
- Eye tracking: Following a moving object smoothly.
- Focusing: Shifting your gaze between near and far objects without strain.
- Convergence: Ensuring both eyes work together as a team.
By improving these foundational visual skills, vision therapy can reduce the strain on your brain, often decreasing the frequency of headaches triggered by reading or screen time.
Cervical Physiotherapy for Neck-Related Symptoms
A significant head injury almost always affects the neck. The upper neck contains many nerves that send signals to the brain about head position. If the muscles and joints in this area are injured, they can send faulty signals that the brain may interpret as a headache or dizziness.
Cervical physiotherapy focuses on these neck issues. A therapist assesses your neck’s range of motion and strength, and may use techniques such as:
- Manual therapy to improve joint movement.
- Specific exercises to strengthen deep neck muscles.
- Postural guidance to reduce daily strain.
For many individuals, addressing the neck is a key component in resolving persistent headaches and dizziness.
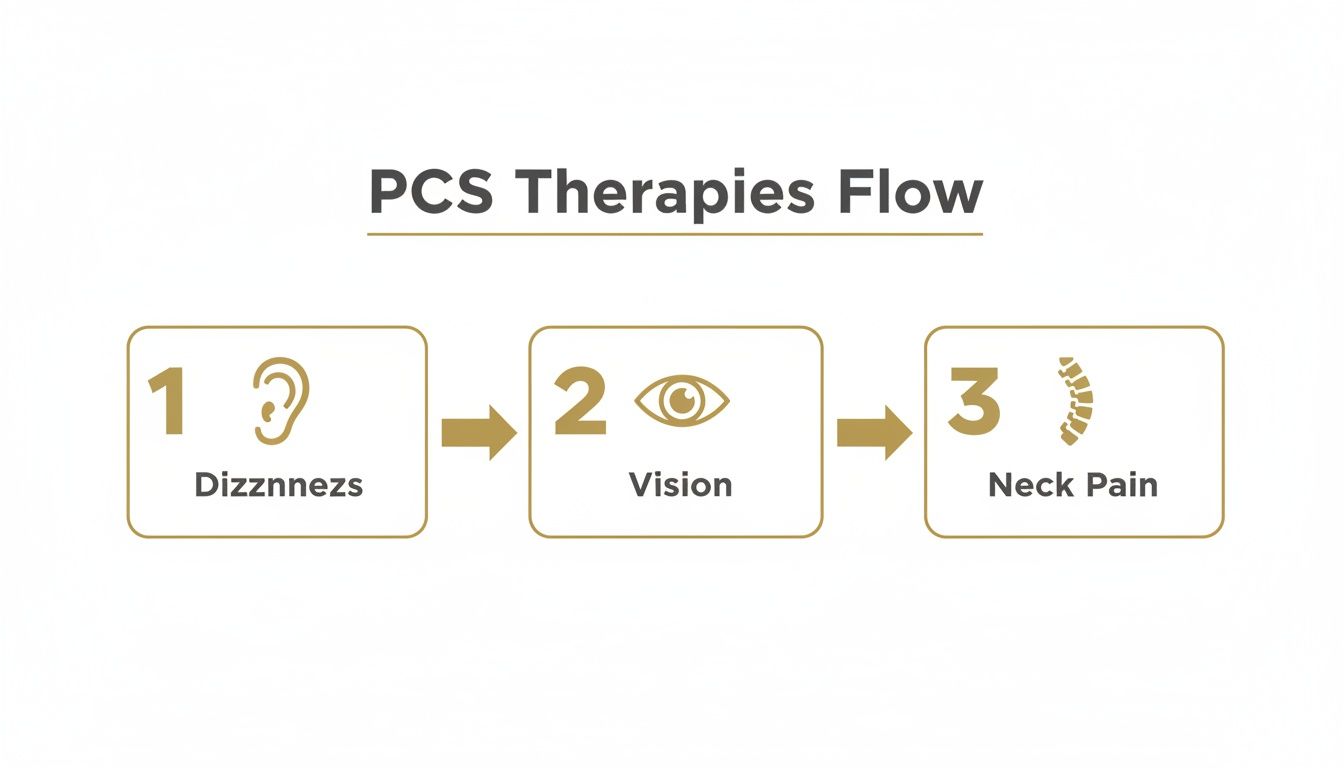
A Summary of Therapeutic Approaches
| Common Symptom | Primary Therapeutic Approach | Goal of Therapy |
|---|---|---|
| Dizziness, Vertigo, Unsteadiness | Vestibular Therapy | To retrain the brain to correctly process signals from the inner ear, improving balance. |
| Headaches, Eye Strain, Light Sensitivity | Vision Therapy | To improve eye tracking, focusing, and coordination, reducing strain on the brain. |
| Neck Pain, Tension Headaches | Cervical Physiotherapy | To restore proper movement and strength in the neck, reducing faulty nerve signals. |
| Anxiety, Low Mood, Overwhelm | Cognitive Behavioural Therapy (CBT) | To develop practical coping strategies for managing symptoms and the emotional impact of recovery. |
As shown, there is a clear logic to how these therapies are applied, each targeting a specific system that has been disrupted by the injury.
Cognitive Behavioural Therapy in Recovery
Living with persistent symptoms can be physically and emotionally draining. It is common to feel frustrated, anxious, or low when recovery takes longer than expected. Cognitive Behavioural Therapy (CBT) is a practical approach that provides tools to manage these challenges.
CBT helps you learn concrete strategies to handle the day-to-day realities of PCS. A therapist can help you:
- Learn to pace yourself and manage your brain’s limited energy.
- Reframe unhelpful thoughts about your recovery.
- Develop coping mechanisms for dealing with brain fog and fatigue.
UK-based research highlights the importance of these active therapies. Studies indicate that early intervention with vestibular and cervical physiotherapy are cornerstones of effective management. You can explore the research on post-concussion syndrome from Cambridge University for more on the clinical perspective.
Understanding how these different therapies work together is a key part of building an effective recovery plan. For a more organised roadmap, our structured Concussion Guide explores these connections in greater detail.
Creating a Gradual Return-to-Activity Plan
Understanding the concept of sub-symptom threshold activity is one thing; applying it day-to-day is another. This is where you begin your active recovery. The goal is to map out a gentle, step-by-step return to daily life, using your symptoms as a guide.
This process is not about pushing through pain. It is about carefully identifying your current limits and then slowly expanding them. A symptom flare-up is not a setback; it is simply feedback. It is your body indicating that a certain activity was too much for that day. You listen, ease back, and try again.
Establishing a Baseline
First, you need to determine your starting point. What can you currently do before your symptoms noticeably worsen? Be honest with yourself.
Your initial plan may seem very simple, and that is perfectly fine. The goal is to begin with activities you know you can manage without triggering a flare-up.
- Cognitive Baseline: Can you read for five minutes before your head begins to ache? Can you focus on a single email for three minutes? That is your starting point.
- Physical Baseline: Can you take a gentle 10-minute walk? Or stand to wash dishes for five minutes? That is where you begin.
These small bursts of activity are the foundation of your recovery. They help demonstrate to your brain that activity itself is not the problem—it is about finding the right dose.
The key is to stop an activity before your symptoms spike. When you finish while still feeling relatively well, you send a powerful message to your nervous system that engagement is safe. This helps break the cycle of fear and avoidance that can complicate recovery.
Once you have found a baseline you can comfortably repeat for several days, you can begin to gently increase the challenge.
A Framework for Progression
Progress should be slow and deliberate. A common clinical approach is to increase either the duration or the intensity of an activity, but not both at the same time.
For example, if your baseline walk is 10 minutes, a sensible progression might look like this:
- Week 1: Maintain a 10-minute walk each day.
- Week 2: Increase the duration to 12 minutes daily.
- Week 3: Keep the walk at 12 minutes, but introduce a slight incline.
The same logic applies to cognitive tasks. If you started with five minutes of reading, you might increase it to seven minutes the following week. This slow, predictable approach allows your brain to adapt without becoming overwhelmed.
As you progress, specific symptoms like dizziness or vision issues may arise, indicating that targeted therapies could be beneficial to help you tolerate more activity.
Managing Common Triggers
Certain environments can be difficult after a concussion because they flood the brain with sensory information. A key part of your plan is learning how to navigate these situations.
Grocery Shops:
Try to visit during quiet, off-peak hours. Wearing sunglasses can reduce the intensity of fluorescent lights, and a cap can help limit peripheral vision to reduce overwhelm. Start with a short list and a brief trip of 10-15 minutes.
Screen Use:
Use blue light filters on all devices. Lowering screen brightness and increasing font size can also reduce eye strain. The 20-20-20 rule is helpful: every 20 minutes, look at something 20 feet away for 20 seconds. Take frequent breaks away from the screen.
Social Gatherings:
Noisy gatherings can be very challenging. Start with one-on-one conversations in a quiet setting. Before attending a busier event, have an exit strategy. This allows you to leave when you feel symptoms increasing, without feeling uncomfortable.
This structured, methodical approach helps put you in control of your recovery. It provides a practical, flexible plan to discuss with your healthcare provider to ensure your progress is safe and steady.
The Role of Medication and Lifestyle in Recovery
While active therapies form the core of post-concussion syndrome treatment, medication and lifestyle choices play important supporting roles. They are best viewed as tools that can make your rehabilitation journey smoother and more effective.
Medication is not typically a first-line treatment for PCS itself. It is rarely used to address the root cause of the condition. Instead, a doctor might prescribe medication to manage a specific, severe symptom that is impeding your progress in rehabilitation.
The goal is to create a window of opportunity for therapy. For example, if severe headaches or insomnia make it impossible to attempt your exercises, a targeted medication might provide enough relief for you to participate. This is a strategic measure to enable healing.
Foundational Lifestyle Factors
After a concussion, the nervous system is in a fragile state. Basic healthy lifestyle habits become essential. They provide the stable, predictable environment your brain needs to repair itself.
Consider these three pillars:
-
Consistent Sleep: Quality sleep is when the brain performs much of its repair work. Poor sleep can amplify nearly every PCS symptom, from headaches to brain fog. Adhering to a consistent sleep-wake schedule and creating a calm bedtime routine can make a significant difference.
-
Steady Nutrition: A concussed brain can struggle to regulate its energy. Blood sugar spikes and crashes may worsen symptoms like cognitive fatigue or irritability. Aim for meals that provide a steady supply of energy by combining protein, healthy fats, and complex carbohydrates. There is also growing evidence for the role of certain nutrients, such as specific Omega-3 fatty acids, in supporting brain health.
-
Stress Management: Living with PCS is inherently stressful. Stress itself consumes the energy your brain needs for healing. Simple, practical techniques like deep breathing or taking a few minutes of quiet time can help calm your nervous system, preserving energy for recovery.
It is important to remember that these lifestyle adjustments support, but do not replace, professional medical advice and active therapies. They work in tandem to create the best possible internal environment for your treatments to be effective.
Navigating the Path to Recovery
Recovery from post-concussion syndrome is best approached as a manageable process, not a search for a single cure. Your most powerful tool is understanding why you are feeling what you are feeling and how different treatments address the underlying issues.
This clarity can change your perspective. It helps you see recovery as a journey with fluctuations, not a straight line. Some days will be better than others. Accepting this rhythm can reduce the frustration that often accompanies a longer healing process. Every small improvement is progress, and a flare-up is simply feedback from your body—not a failure.
When to Seek Further Medical Advice
While taking an active role is key, it is also important to know when to consult your GP or specialist. You should seek medical advice if you notice:
- A sudden and severe worsening of your symptoms, such as a headache that is much worse than usual.
- The appearance of new neurological signs, such as weakness in your limbs, numbness, or difficulty with speech.
- A lack of improvement in your symptoms despite consistently following your active recovery plan.
These are signals that a closer evaluation may be needed to adjust your treatment plan.
From Understanding to Action
When you have clarity, confusion gives way to purposeful action. In the UK, research has shown that early intervention based on education and reassurance can be highly effective. In fact, studies suggest that even a single session focused on explaining symptoms and setting realistic expectations can significantly reduce the long-term impact of PCS. You can read more about the findings on early psychological interventions in Great Britain.
This principle is central to recovery: a structured, informed approach is what moves you forward. Articles like this are a good starting point for building your understanding, but a well-organised recovery often benefits from a more connected roadmap.
That is why we created our comprehensive guides. They are a logical next step for those who want to move beyond individual articles and develop a detailed, step-by-step plan. They take these concepts and weave them into a deeper, structured framework to support your recovery.
Frequently Asked Questions About PCS Recovery
It is normal to have many questions when navigating post-concussion syndrome, especially when recovery seems unpredictable. Here, we address some of the most common concerns to provide clarity and help you set realistic expectations.
How Long Does Post-Concussion Syndrome Last?
There is no single timeline for recovery; it varies for each individual. Many people see significant improvement within three to six months, but it is not uncommon for symptoms to persist for a year or longer.
Factors that can influence recovery time include the severity of the initial injury, pre-existing conditions like migraines or anxiety, and the consistency of your rehabilitation plan. It is often more helpful to focus on small, steady improvements rather than a fixed end date. This mindset can make the process less frustrating.
Can I Exercise with Post-Concussion Syndrome?
Yes, gentle, controlled exercise is now considered a key part of recovery. This is a shift away from the old advice of complete rest. The approach is known as sub-symptom threshold exercise.
The goal is to slightly elevate your heart rate without triggering a significant increase in symptoms. Light aerobic activities like walking or using a stationary bike can help restore proper blood flow to the brain and calm the autonomic nervous system. It is important to start slowly and increase the duration or intensity only with guidance from a professional, such as a physiotherapist with experience in concussion management.
Why Do Screens and Busy Places Make Symptoms Worse?
This is a very common experience for people with PCS. After a concussion, the brain's ability to filter and process sensory information is often temporarily impaired.
Think of your brain’s processing capacity as being reduced.
- Screens: The bright light and focused attention required for computers and phones can quickly overwhelm the visual system. It is like trying to run complex software on an older computer—it drains the available resources quickly.
- Busy Environments: A supermarket, for example, presents a sensory overload. Your brain must simultaneously process bright lights, numerous sounds, and constant movement. This overload can trigger headaches, dizziness, or intense brain fog.
To manage this, you can use screen filters, take frequent breaks (the 20-20-20 rule), and gradually re-introduce yourself to busy environments for short, planned periods. Each successful exposure helps your brain rebuild its tolerance.
At The Patients Guide, we create structured resources that bring this level of clarity to your entire health journey. For a more organised path forward, explore our full library of patient guides.
Also in News

Your Guide To Understanding Back and Leg Pain
January 29, 2026 13 min read
Struggling with back and leg pain? Our guide explains the common causes, how clinicians diagnose the issue, and the paths to finding relief.
Read More
When Is the Best Time to Take Magnesium? A Guide to Timing Your Supplement
January 28, 2026 8 min read
Discover the best time to take magnesium for sleep, energy, or general health. Our guide explains how timing and type affect absorption and effectiveness.
Read More
Understanding Brain Fog Symptoms and Finding Clarity
January 27, 2026 11 min read
A calm, clear guide to understanding brain fog symptoms. Learn the common signs, potential causes, and practical next steps for managing mental fatigue.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
