Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
Understanding Frozen Shoulder Treatment: A Clear Guide
January 31, 2026 13 min read
Dealing with the pain and stiffness of a frozen shoulder can be a frustrating experience. Searching for answers online often leads to conflicting advice, leaving you unsure of the best path forward. Many people find themselves trying different things without a clear understanding of why.
This guide is designed to reduce that confusion. We will explain how healthcare professionals think about frozen shoulder, moving beyond a simple list of tips to help you understand the condition itself.
Our goal is to provide a calm, clear overview of what is happening in your shoulder, the typical stages of recovery, and the treatments that are most appropriate at each point. This is not about miracle claims; it is about providing the clarity needed to navigate your treatment with confidence.
What is Happening Inside the Shoulder?

The clinical term for frozen shoulder is adhesive capsulitis. This name provides a useful clue about what is happening. Your shoulder joint is enclosed in a flexible tissue called the capsule. With a frozen shoulder, this capsule becomes inflamed, thickens, and tightens.
Think of the capsule as a loose, elastic covering that allows your arm to move freely. When adhesive capsulitis occurs, this covering starts to shrink and develops stiff bands of tissue known as adhesions. It is this physical tightening that restricts movement and causes significant pain.
This process typically follows a predictable, three-stage pattern.
The Three Stages of Frozen Shoulder
Understanding these stages is important because the most effective frozen shoulder treatment often depends on which phase you are in.
| Stage | Typical Duration | Primary Symptoms |
|---|---|---|
| Stage 1: Freezing | 2 to 9 months | Pain is the dominant symptom, often sharp and worse at night. Range of motion becomes progressively more limited. |
| Stage 2: Frozen | 4 to 12 months | Stiffness becomes the primary issue. Pain may lessen, but the shoulder feels extremely restricted. |
| Stage 3: Thawing | 6 months to 2+ years | Range of motion gradually and steadily improves as the shoulder "thaws." |
Identifying your current stage helps clinicians tailor treatment to be as effective as possible.
Why an Accurate Diagnosis Matters
A correct diagnosis is the critical first step. A healthcare professional will assess your shoulder's movement against established shoulder range of motion norms. They evaluate both your active range (how you move the arm yourself) and passive range (how far they can move it for you) to confirm the joint capsule is the source of the restriction.
In the UK, frozen shoulder is a common condition. Research indicates that 8.2% of men and 10.1% of women may experience it at some point, causing significant disruption to daily activities.
While recovery can feel slow, the long-term outlook is generally positive. One study following patients for over four years found that 59% regained normal or near-normal shoulder function. Only a small percentage, 6%, experienced severe, long-term issues.
A diagnosis of frozen shoulder is not just a label for a painful, stiff shoulder. It describes a specific pathological process within the joint capsule itself. This distinction is critical because it guides the entire treatment strategy, ensuring that interventions are matched to the underlying problem.
The Foundation: Physiotherapy and Self-Care

For most people, physiotherapy and thoughtful self-care form the bedrock of frozen shoulder treatment. These conservative approaches focus on managing pain and gently restoring movement without aggravating the underlying inflammation.
The goal is not to force the shoulder through pain. It is a careful process of encouraging the stiffened joint capsule to gradually release its grip. In clinical settings, this partnership is key: the physiotherapist provides expert guidance, while consistent effort at home drives progress. For many, this is sufficient to navigate the stages of the condition.
The Role of a Physiotherapist
A physiotherapist acts as a guide, first assessing your specific stage and degree of motion loss. They then create a tailored programme.
This guidance is crucial. A common mistake, particularly in the painful 'freezing' stage, is pushing too hard, too soon. This can increase inflammation and cause a setback. A physiotherapist helps you find the balance between a helpful stretch and a harmful strain.
Core Principles of Movement and Stretching
The prescribed exercises have specific goals that evolve as the shoulder heals.
Initially, the focus is on gentle range-of-motion exercises. The main objective is to prevent further stiffening and maintain existing movement. These are often passive movements, where the unaffected arm or gravity provides the force, not the muscles of the injured shoulder.
Later, in the 'thawing' stage, as pain subsides, the focus shifts. Exercises become more active, aiming to regain lost mobility and rebuild strength in the supporting shoulder muscles.
It is a common misconception that physiotherapy for a frozen shoulder must be aggressive to be effective. The opposite is often true. Successful approaches are built on patience and persistence, working with the shoulder's limits, not against them. Gentle, consistent movement is what encourages the joint capsule to loosen.
Foundational Exercises for Early Stages
Here are two classic exercises often recommended in the initial phase. They are designed to be low-impact and encourage movement without force.
-
Pendulum Swings: Lean over a sturdy table, supporting yourself with your good arm. Allow the affected arm to hang down. Use your body's momentum to gently swing the arm in small, slow circles. The shoulder muscles should remain relaxed; gravity does the work.
-
Finger Walks: Stand facing a wall, about an arm’s length away. Place the fingertips of your affected arm on the wall. Slowly 'walk' your fingers up the wall, going only as high as is comfortable without sharp pain. Hold briefly, then slowly walk them back down.
Learning how to treat frozen shoulder at home with the correct techniques is a significant part of the recovery process.
Practical Self-Care Strategies
Daily habits can significantly impact pain levels and recovery speed.
-
Pain Management: Applying a warm pack to your shoulder for 10-15 minutes before stretching can help relax tight tissues. After exercise, if the shoulder feels sore, an ice pack can help reduce any inflammation.
-
Activity Modification: Be mindful of movements that trigger sharp pain, such as reaching quickly overhead or behind your back. Adapt your environment, for example, by moving frequently used kitchen items to lower, more accessible shelves.
-
Sleeping Position: This is often a major factor. Avoid sleeping on the painful shoulder. Lying on your back with a pillow under the affected arm for support can be helpful. Alternatively, sleep on your good side while hugging a pillow to support the affected arm.
The neck and shoulder are closely connected, so managing tension in one area may help the other. Our guide with simple exercises for neck pain relief may also be useful.
Medical Interventions for Pain Relief
During the initial 'freezing' stage, pain can be persistent and may disrupt sleep, making physiotherapy seem impossible. When pain is too severe to allow for gentle exercises, medical interventions can play a crucial role.
The purpose of these treatments is not to provide an instant cure. The primary focus is to reduce the intense inflammation within the joint capsule, which is the source of the pain. By interrupting the pain cycle, these interventions can create a window of opportunity for physiotherapy to become effective.
Medication to Reduce Pain and Inflammation
The first step is often simple. Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be effective in reducing both pain and inflammation. When taken as guided by a GP or pharmacist, they may be sufficient to make daily activities more manageable and allow for stretching exercises.
If over-the-counter options are not enough, a doctor may prescribe stronger anti-inflammatory medication for a short period. The objective remains the same: to calm the shoulder enough to begin the important work of restoring movement.
Corticosteroid Injections: A Targeted Approach
When oral medications are insufficient, a corticosteroid injection is often considered. This involves injecting a powerful anti-inflammatory medicine directly into the shoulder joint.
The procedure is quick and typically performed in a clinic. It delivers a concentrated dose of medication directly to the inflamed and tightening joint capsule.
The primary benefit of a steroid injection is often significant pain relief, particularly in the first few weeks to months. This can create an ideal period to work with a physiotherapist to improve range of motion.
It is helpful to view the injection as a tool, not a standalone cure. It helps to reduce pain so that the real work of stretching and movement can begin. Some people also find that exploring supplements that support joint health can be a useful component of their overall recovery plan.
A Look at Clinical Practice in the UK
In the UK, clinicians typically follow a measured, stepwise approach. A survey of shoulder specialists revealed that in the early, painful stage, about one-third recommend starting with education and oral pain relief, while another third suggest beginning with physiotherapy.
Notably, only 18% advise an intra-articular steroid injection as the very first treatment. This indicates a common preference for trying less invasive options first. You can discover more insights about these treatment pathways on boa.ac.uk.
What Is Hydrodistension?
You may also hear a specialist mention hydrodistension (also known as a high-volume injection or hydrodilatation). This procedure is similar to a standard injection but involves a larger volume of fluid—typically a combination of saline, local anaesthetic, and a steroid.
The goal is twofold. First, the steroid addresses the inflammation. Second, the volume of the fluid is intended to physically stretch the tight joint capsule from the inside, potentially breaking down some of the adhesions that are restricting movement.
Hydrodistension is usually performed using ultrasound guidance to ensure accuracy. It is often considered when stiffness is the primary problem and a standard steroid injection has not provided the breakthrough needed to progress with physiotherapy.
Procedures for Persistent Stiffness
Most cases of frozen shoulder resolve with time and consistent physiotherapy. However, if months of effort result in a frustrating plateau where severe stiffness persists, it may be time to discuss next-level procedures with a specialist.
This is a significant decision, typically reserved for when conservative treatments have not provided sufficient relief. The goal of these procedures is to physically release the tight joint capsule, creating an opportunity for a substantial improvement in movement that must be maintained with focused physiotherapy.
Manipulation Under Anaesthesia (MUA)
Manipulation Under Anaesthesia (MUA) is a non-surgical procedure performed by an orthopaedic surgeon. While you are under general anaesthesia, the surgeon carefully moves your arm through its full range of motion.
This controlled movement is designed to stretch and tear the adhesions that have formed within the joint capsule. Because the surrounding muscles are completely relaxed, the surgeon can achieve a release that would be impossible otherwise. The procedure is brief, and patients typically go home the same day.
The real work begins immediately after the MUA. Its success is highly dependent on starting an intensive physiotherapy programme right away to maintain the newly gained movement and prevent the capsule from stiffening again.
Arthroscopic Capsular Release (ACR)
Arthroscopic Capsular Release (ACR) is a minimally invasive 'keyhole' surgery. The surgeon makes a few small incisions around the shoulder.
A small camera (arthroscope) is inserted through one incision, providing a clear view of the joint's interior on a monitor. Specialised instruments are used through the other incisions to precisely cut and remove the thickened parts of the joint capsule. This directly addresses the structures blocking movement.
ACR is often considered for particularly resistant cases or when MUA may not be appropriate. As with MUA, post-procedure physiotherapy is essential for a successful outcome. An accurate diagnosis is also vital, as conditions like a rotator cuff tear can sometimes present with similar symptoms. You can learn more in our guide on rotator cuff tear symptoms and treatments.
Comparing Advanced Frozen Shoulder Treatments
When symptoms do not improve, a specialist may discuss MUA or ACR. While both aim to restore movement, they work differently. This table outlines the key differences.
| Treatment | How It Works | Best Suited For | Key Consideration |
|---|---|---|---|
| Manipulation Under Anaesthesia (MUA) | The surgeon manually stretches and tears the tight joint capsule while the patient is under general anaesthesia. | Patients in the 'frozen' stage whose primary issue is stiffness and who have not responded to injections or physiotherapy. | Non-surgical, but the release is less controlled. Immediate, intensive physiotherapy is non-negotiable for success. |
| Arthroscopic Capsular Release (ACR) | A surgeon uses keyhole surgery to directly view and precisely cut the thickened joint capsule. | People with very severe, persistent stiffness, or when other conditions inside the joint need to be addressed. | More invasive, but the release is very precise. Allows the surgeon to inspect the joint for any other issues. |
Ultimately, both MUA and ACR can be effective. The choice often depends on the specifics of your case and a shared discussion with your surgeon about the potential benefits and risks.
Making an Informed Choice
Deciding on a procedure is a conversation with your healthcare team. There is no single ‘right’ answer for everyone.
The United Kingdom Frozen Shoulder Trial (UK FROST) compared three approaches: Early Structured Physiotherapy, MUA, and Arthroscopic Capsular Release. The results showed that all three groups experienced significant improvements, but no single treatment was found to be clearly superior. You can read the full research about these trial findings.
This suggests that the "best" treatment is the one that fits your specific situation, based on the stage of your condition and a discussion with your specialist. Both MUA and ACR carry the standard risks of any procedure involving anaesthesia, which your surgeon will review with you in detail.
Long-Term Recovery and Shoulder Health
Recovering from a frozen shoulder is a marathon, not a sprint. The final ‘thawing’ stage can feel slow, but this is where patience and consistency make a significant difference. Understanding what to expect during healing and how to care for your shoulder long-term is key to a lasting recovery.
The timeline varies for each person. While the thawing stage can last from six months to over two years, the goal is steady, gradual progress. It is helpful to focus on small improvements—like being able to reach a high shelf without thinking—rather than becoming discouraged by the pace.
The Importance of a Maintenance Programme
Once you feel better, it can be tempting to stop your exercises. However, transitioning to a ‘maintenance programme’ is one of the most important steps you can take. This does not mean continuing a full physiotherapy routine indefinitely.
It involves incorporating a few key stretches and strengthening exercises into your week. This helps maintain the flexibility you regained and ensures the supporting muscles remain strong.
A simple maintenance plan could include:
- Continued Stretching: A few times a week, perform the main range-of-motion stretches that were most helpful.
- Strength Maintenance: Continue with light resistance exercises for the rotator cuff and shoulder blade muscles.
- Mindful Movement: Pay attention to posture and how you move throughout the day to avoid unnecessary strain on the joint.
Can Frozen Shoulder Return?
This is a common question in clinical practice. The good news is that it is very rare for a frozen shoulder to recur in the same shoulder. The specific inflammatory process that causes the capsule to stiffen does not usually happen in the same joint twice.
However, it is more common to develop a frozen shoulder in the opposite shoulder, sometimes within about five years. This is not guaranteed, but it highlights the importance of managing overall health and any contributing risk factors, such as diabetes.
Following a procedure like MUA or Arthroscopic Capsular Release, your post-operative physiotherapy is vital. This structured rehabilitation allows you to maximize your newly restored movement and prevents the shoulder from stiffening again as it heals.
For readers wanting a structured overview of shoulder care, our library of shoulder patient guides explores these topics in more detail.
Making Sense of Your Treatment Plan
We have covered the stages of frozen shoulder and the spectrum of available treatments. A key takeaway is that there is no single ‘best’ frozen shoulder treatment. The right path depends on your specific symptoms, your stage of recovery, and your goals.
This guide is intended to provide a map, not a set of rigid instructions. Understanding the reasoning behind your clinician's recommendations allows you to be an active participant in your recovery. The aim is to move from feeling confused to feeling informed and in control.
Visualising Your Path Forward
A comprehensive recovery plan looks beyond immediate pain relief to long-term shoulder health. This flowchart illustrates how the journey typically progresses from active treatment to maintenance and prevention.
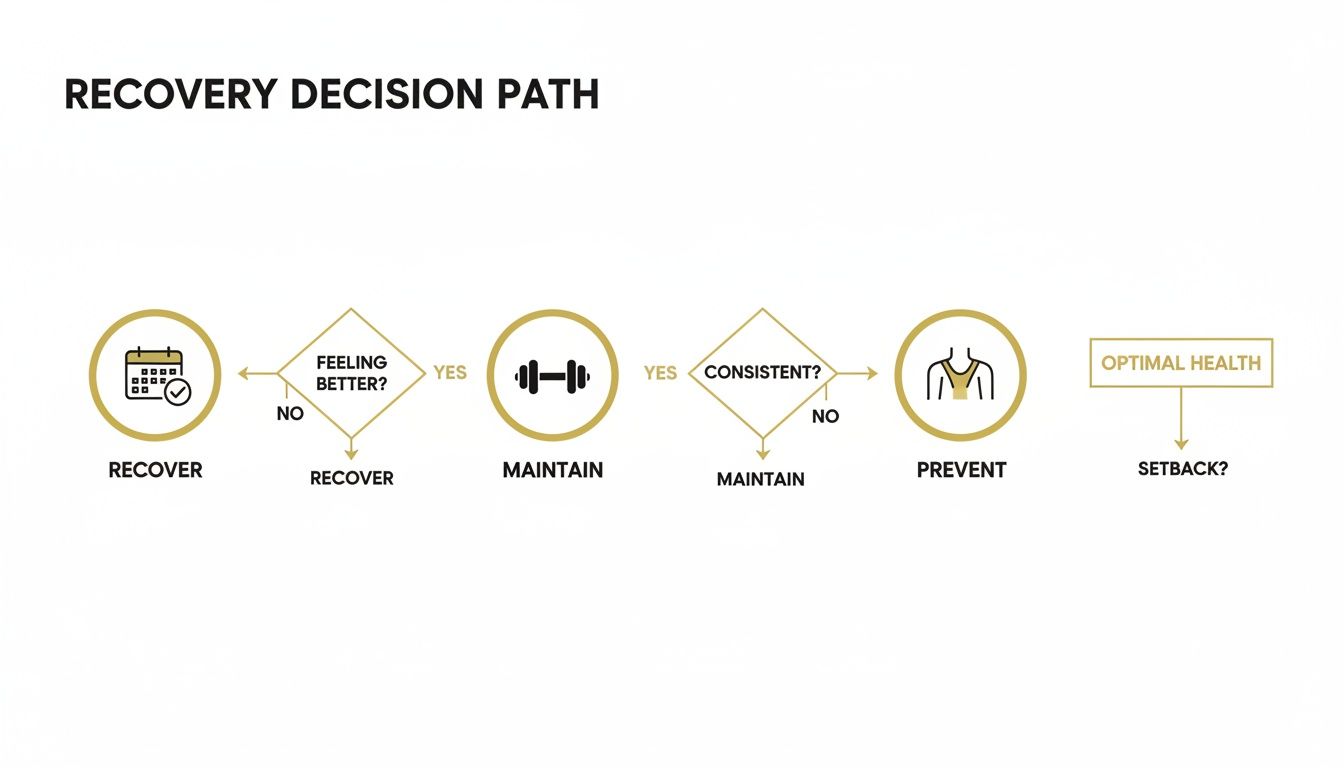
The journey does not end when the worst of the pain subsides. It transitions into a phase focused on maintaining good movement and rebuilding strength. Your treatment plan should be a living document that evolves as you progress.
The best treatment plans are always a partnership. Your day-to-day experience and understanding of your own body are just as crucial as your healthcare provider's clinical expertise.
When you have clarity, you can ask better questions and feel more confident in the decisions you make. Understanding why a certain exercise is recommended or what an injection is intended to achieve helps you commit to your recovery. For many, this shift in perspective is a turning point.
From Understanding to Action
While an article is a good starting point, sometimes a more organised framework is needed to apply this knowledge.
If this overview has been helpful and you are looking for a more structured next step, our guides are created for people who want clarity beyond blogs. They connect these concepts into a clear, step-by-step path, providing well-organised information for the journey ahead.
Your Questions About Frozen Shoulder Answered
Here are answers to a few of the most common questions about frozen shoulder treatment.
How Long Does a Frozen Shoulder Usually Last?
There is no single timeline, but most cases of frozen shoulder resolve over 1 to 3 years. The condition moves through three distinct phases: 'freezing' (painful), 'frozen' (stiff), and 'thawing' (recovery).
The duration of each stage varies from person to person. While this timeframe may seem long, treatment aims to manage symptoms and potentially shorten the overall process.
Can I Treat Frozen Shoulder on My Own?
A home exercise programme is central to recovery, but it is best not to develop one without professional guidance, at least initially. A proper diagnosis from a physiotherapist or GP is important.
A professional can confirm that it is a frozen shoulder and not another condition. They can also provide a safe, structured exercise plan appropriate for your current stage and advise if other interventions, like a steroid injection, may be beneficial.
What Should I Avoid with a Frozen Shoulder?
The main principle is to avoid sudden, jarring, or forceful movements. Pushing through sharp pain is likely to increase inflammation and can be a setback.
Gentle stretching should only be taken to the point of a mild, deep stretch, never sharp pain.
Other things to avoid include:
- Lifting heavy objects with the affected arm.
- Painful overhead activities that strain the joint.
- Sleeping on the affected shoulder, as this prolonged pressure can increase pain.
The key is to keep the shoulder moving within a comfortable, safe range.
Is There a Link Between Diabetes and Frozen Shoulder?
Yes, a strong connection exists. People with diabetes have a significantly higher risk of developing frozen shoulder—up to five times higher than those without diabetes. The condition also tends to be more severe and resistant to treatment in this group.
The exact reason for this link is not fully understood, but a leading theory suggests that elevated blood sugar levels can affect the collagen in the shoulder capsule. This may cause collagen fibres to become stiff and 'sticky,' contributing to the tightening that defines frozen shoulder.
Therefore, maintaining good blood sugar control is not only important for overall health but may also play a role in shoulder recovery.
At The Patients Guide, our goal is to help you move from confusion to clarity. For those who want to go beyond articles and build a structured understanding of their health, our guides offer a clear, step-by-step path forward. Explore our full library to take control of your health journey.
Also in News

A Calm Guide to Treating Whiplash at Home
February 10, 2026 10 min read
Feeling overwhelmed by neck pain after an injury? This is a calm, clear guide to treating whiplash at home, focusing on safe pain relief and recovery.
Read More
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
