Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
Understanding Back Pain When Breathing
February 01, 2026 13 min read

Feeling a sharp pain or a persistent ache in your back each time you breathe can be unsettling. It’s the kind of symptom that often leads to confusing and contradictory online searches, leaving you more worried than when you started.
Many people experience this, and the uncertainty is a common part of the process. This article is designed to provide clarity by explaining how healthcare professionals think about this symptom.
The goal isn't to give you a diagnosis, but to help you understand the possible reasons for the pain, from the most common mechanical issues to the less common medical conditions that require attention. Understanding the framework clinicians use can help reduce confusion and prepare you for a more productive conversation with your doctor.
Understanding the Sources of Breathing-Related Back Pain
The first step in a clinical setting is to categorise the potential causes. This systematic approach helps narrow down the possibilities logically, starting with the most frequent and straightforward issues before considering more complex conditions.
This structured thinking helps make sense of a confusing symptom.
Common Areas of Concern
When a professional assesses back pain linked to breathing, they typically consider three main areas: the muscles and skeleton, inflammatory conditions, and issues related to internal organs.
Here is a simplified overview of how these categories are often broken down:
Quick Guide to Potential Causes of Back Pain When Breathing
| Category | Common Examples | Typical Pain Description |
|---|---|---|
| Musculoskeletal Issues | Pulled intercostal muscle, rib injury, spinal joint dysfunction. | Sharp, localised, and reproducible with specific movements or pressure. |
| Inflammatory Conditions | Pleurisy (inflamed lung lining), costochondritis (inflamed rib cartilage). | Sharp, stabbing pain, often worse with a deep breath or cough. |
| Internal Organ Problems | Lung infections (pneumonia), gallbladder issues, kidney problems. | Deeper, more constant ache that may not change with position. |
This method helps distinguish between different types of problems. For instance, if the pain also travels down the leg, it suggests a different set of potential causes, which we explore in our guide to understanding back and leg pain.
Thinking in these clear categories helps replace anxiety with a more logical perspective on what may be happening.
The Mechanical Link Between Breathing and Back Pain
To understand why a simple breath can cause back pain, it’s helpful to view your torso as a single, interconnected system. This system includes your spine, rib cage, diaphragm, and the small intercostal muscles between your ribs.
When you inhale, your diaphragm—the large, dome-shaped muscle at the base of your lungs—contracts and moves downward.
Simultaneously, your intercostal muscles lift your rib cage up and outward. This coordinated movement creates space for your lungs to expand. It’s a subtle motion, but it occurs thousands of times every day.
How Simple Movement Creates Pain
Imagine your rib cage moving like the handle on a bucket. With each breath, the handle (your ribs) rises and falls. If a muscle is strained, a joint is inflamed, or a hinge is stiff, this repetitive movement can irritate an already sensitive area.
This is the core mechanical reason for back pain when breathing. The underlying issue doesn't have to be severe; it just needs to be located in the path of this constant motion.
This concept map helps illustrate how various problems, from simple strains to more complex conditions, can all result in pain during respiration.
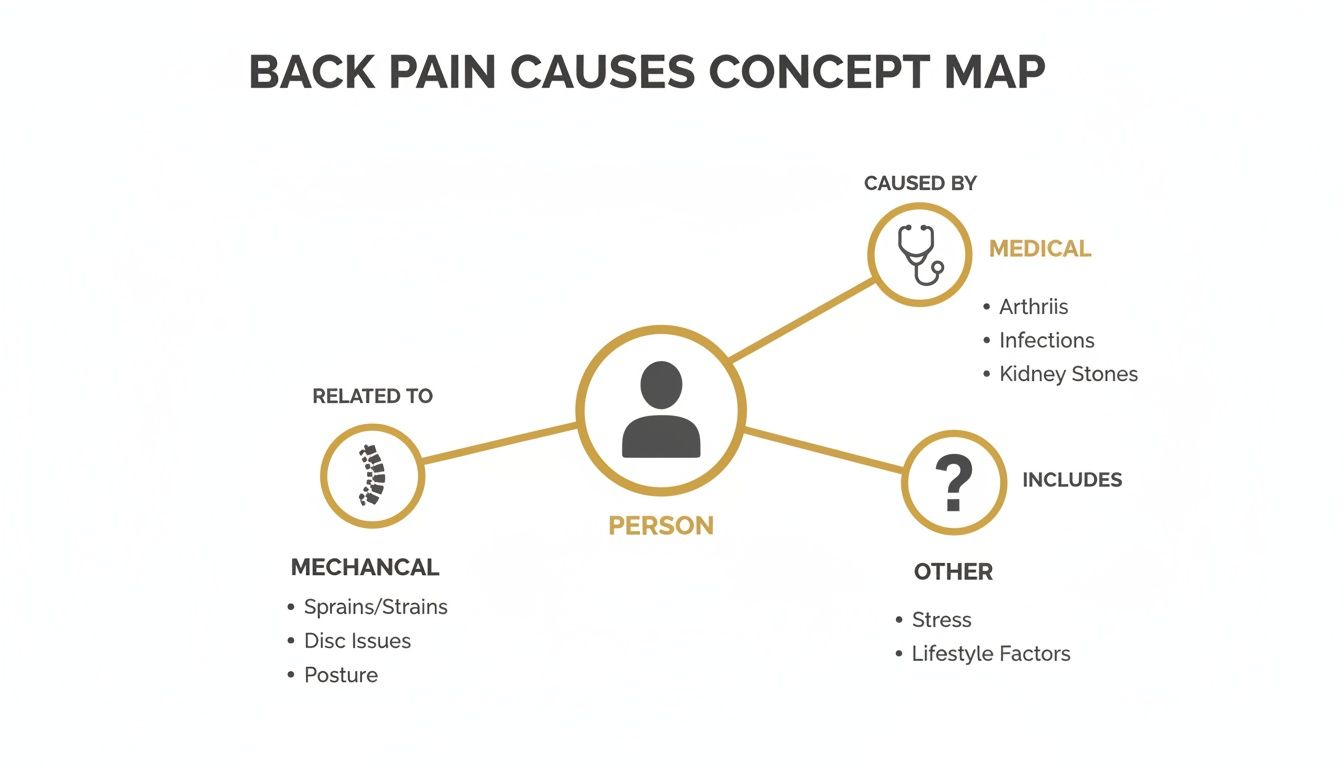
As you can see, while serious medical issues are a possibility, everyday mechanical problems in the spine and ribs are a common cause of this specific type of pain.
The Role of Your Diaphragm and Core
Your diaphragm is not just a breathing muscle; it’s also a key component of your core stability. It attaches directly to your lower ribs and even to the vertebrae of your lumbar spine (your lower back).
When breathing patterns are disrupted—often due to stress, poor posture, or an old injury—other muscles must compensate. These accessory breathing muscles, which include muscles in your neck, shoulders, and upper back, are not designed for this constant workload.
In clinical settings, we often see individuals who rely heavily on their neck and shoulder muscles for normal breathing. This can create a cycle of chronic tension in the upper back, which becomes painful with the stretch of a deep inhalation.
Relying on these smaller, less efficient muscles can lead to fatigue, strain, and persistent knots that are easily aggravated by the simple act of breathing.
Why Posture Is a Major Factor
Poor posture, particularly slouching, can significantly disrupt breathing mechanics. Hunching forward compresses the front of the rib cage and forces the joints of the thoracic spine (mid-back) into a stiff, rounded position.
This makes it physically more difficult for the ribs to expand properly. When you attempt to take a deep breath, you are forcing movement in joints that have become restricted and muscles that are already under strain. The result is often a sharp pain at the site of the problem.
Learning proper breathing mechanics is important for core stability and can make a significant difference. Exploring practices like breathing techniques for Pilates can be a useful starting point, as they focus on engaging the diaphragm and expanding the rib cage correctly.
When a clinician assesses back pain that worsens with breathing, the first area they typically investigate is the musculoskeletal system—the network of muscles, bones, and joints. While the sensation can be alarming, this type of pain most often stems from a mechanical issue rather than a more serious internal condition.
A key indicator is that the pain is usually localised. You can often point to the exact spot that hurts, and specific movements or direct pressure will reproduce the pain. This strongly suggests the problem lies within the structure of your back or chest wall, not your organs.

Intercostal Muscle Strain
One of the most common causes is a strain of the intercostal muscles. These are the small muscles running between your ribs, responsible for expanding and contracting your chest as you breathe. Like any muscle, they can be pulled or strained.
This can happen from a sudden movement, such as a forceful cough, a sneeze, or twisting awkwardly. It can also develop gradually from repetitive tasks or poor posture that places continuous strain on the rib cage.
The pain is typically sharp and localised to a specific spot. It tends to worsen significantly with a deep breath, cough, or laugh, as these actions stretch the injured muscle fibres. The area is also likely to be tender to the touch.
Costochondritis and Rib Joint Issues
Another common diagnosis is costochondritis, an inflammation of the cartilage connecting the ribs to the breastbone. Although the inflammation is at the front of the chest, the pain can radiate to the back, which can be confusing.
This condition often causes a sharp, aching pain that can mimic heart-related issues. For a clinician, a key diagnostic sign is tenderness upon pressing specific rib joints next to the breastbone.
A similar issue can occur at the back, where the ribs attach to the spine (the costovertebral and costotransverse joints). If these joints become irritated or stiff, it can create a deep, nagging ache in the back that is provoked by the movement of breathing.
In a clinic, distinguishing between these conditions often comes down to a careful physical examination. Locating the precise point of tenderness—whether between the ribs, at the front near the sternum, or next to the spine—provides crucial clues to identify the mechanical fault.
Thoracic Spine Dysfunction
The thoracic spine (your mid and upper back) is designed for stability, but it must also allow for subtle movement with each breath. If the joints in this area become stiff or dysfunctional, it is a very common source of pain when breathing.
When these spinal joints become "stuck," often due to prolonged slouching or a minor injury, the rib cage cannot expand freely. Taking a deep breath forces these stiff joints to move, which can result in a sharp pain or a deep ache.
This is a significant issue, particularly in workplace settings. Between 2018 and 2019, an estimated 498,000 UK workers suffered from work-related musculoskeletal disorders. Factors like poor desk ergonomics and heavy lifting are major contributors to back and intercostal strains that can make breathing uncomfortable.
How We Tell It's Musculoskeletal Pain
To determine if pain is musculoskeletal, clinicians look for several patterns:
- Is the pain reproducible? Can the pain be consistently triggered by pressing on a specific spot or performing a particular movement, like twisting or bending?
- Is it mechanical? Does the pain change with posture? For example, does it improve when lying down but worsen when sitting?
- Is there a recent injury? Did the pain begin after a fall, an awkward movement, or a bout of intense coughing?
If you have experienced a direct injury to your ribs, our guide to managing a bruised rib offers specific information. For most musculoskeletal issues, the outlook is generally very good with appropriate care, even if the pain is intense initially.
While many aches that worsen with breathing are related to muscle strains, it is important to recognise symptoms that may indicate a more serious issue. This is not about causing alarm, but about being informed and knowing when to seek professional medical advice.
In clinical practice, certain signs are referred to as "red flags." These are symptoms that suggest a condition may need prompt medical evaluation.
When to Seek Urgent Medical Care
Your lungs, heart, and major blood vessels are all located within your chest cavity. Sometimes, a problem with one of these vital organs can manifest as pain felt in the back. For this reason, certain symptoms should not be ignored.

You should seek immediate medical help if your back pain is accompanied by any of the following:
- Severe, sudden, or crushing chest pain: A sensation of intense pressure or squeezing in your chest is a major warning sign.
- Pain spreading to your arm, jaw, or shoulder: This is a classic pattern that can be associated with a heart attack.
- Significant shortness of breath: Difficulty catching your breath, especially while at rest, is a serious symptom.
- Fever, chills, or coughing up blood: These could be signs of an infection like pneumonia or another significant lung issue.
- Sudden weakness or numbness: Pay close attention if this affects one side of your body, your legs, or your groin area.
These symptoms warrant an urgent evaluation to rule out conditions like a heart attack, a pulmonary embolism (a blood clot in the lung), or a severe infection.
A core principle in medicine is to first investigate and rule out the most serious potential causes. When someone presents with symptoms like severe chest pain and breathlessness, the immediate priority is a rapid and thorough assessment in an emergency setting.
Other Important Signs to Discuss with Your Doctor
Beyond emergencies, other symptoms warrant a prompt conversation with your GP. These signs suggest something may require further investigation, but they do not typically require an emergency visit.
Make an appointment if your back pain is accompanied by:
- Unexplained weight loss: Losing a noticeable amount of weight without changes to your diet or exercise routine can sometimes indicate a systemic issue.
- A history of cancer: Any new or unusual back pain should always be discussed with your medical team.
- Pain that is constant and worse at night: Musculoskeletal pain often changes with position. Relentless pain may be a clue to something else.
- Feeling generally unwell: Vague but persistent feelings of illness alongside the pain are worth mentioning.
A condition like pleurisy, for instance, involves inflammation of the lining around the lungs. It causes a sharp, stabbing pain in the chest and back when breathing and often follows an infection. You can learn more in our detailed guide on pleurisy.
Knowing the difference between these types of symptoms is empowering. It helps you feel more confident managing minor strains at home while also knowing when it is appropriate to seek professional help.
How Clinicians Get to the Bottom of Back Pain with Breathing
When you present to a clinic with back pain when breathing, a doctor or physiotherapist begins a methodical investigation. This is a structured process designed to narrow down the possibilities and identify the most likely cause.
Understanding this process can demystify the appointment and help you feel more like an active participant in your own care. The clinician’s job is to fit the pieces of the puzzle together—your history, the physical examination, and any necessary tests—to form a clear picture.
It All Starts with Your Story
The first and often most revealing step is the clinical history. Your healthcare provider will ask a series of specific questions to build a detailed picture of your experience. This conversation is the foundation of the diagnostic process.
They are trying to understand the "personality" of your pain. Expect questions like:
- The Onset: When did it start? Was it a sudden event, or did it develop gradually?
- The Location: Can you point to the exact spot that hurts? Does the pain radiate elsewhere?
- The Sensation: How would you describe the pain? Is it sharp, dull, aching, or burning?
- The Triggers: Besides breathing, what makes it worse? Coughing? Sneezing? Twisting?
- The Context: Have you been unwell recently? Have you had any injuries? Have you started a new physical activity?
This initial conversation helps the clinician begin to categorise the possibilities, often pointing them toward either a musculoskeletal issue or something requiring further investigation.
The Hands-On Physical Examination
Following the history, the clinician will perform a physical examination. This is a hands-on assessment to confirm suspicions and gather more objective information. It is not just about finding what hurts, but also about what doesn't.
During the exam, they will likely:
- Watch you breathe: They will observe the movement of your chest and abdomen to check for any strained or unusual patterns.
- Gently press on the area (palpation): They will use their fingers to carefully assess different parts of your back, ribs, and spine to locate tender spots.
- Check your movement: You may be asked to bend, lean, and twist to see how these movements affect the pain.
- Listen to your lungs: Using a stethoscope, they will listen for any signs of infection or inflammation within your lungs.
From a clinical perspective, a key moment is when we can reproduce the patient's exact pain just by pressing on a specific rib joint or muscle. This is a huge clue that the cause is mechanical—related to the body's structure—rather than an internal organ.
This hands-on approach provides valuable information that imaging alone cannot offer. It helps differentiate a simple muscle strain from a more complex joint problem or a condition that warrants further tests.
Deciding If Further Tests Are Needed
In many cases, the history and physical exam provide a clear indication of the cause. If a diagnosis like an intercostal muscle strain seems highly probable, further tests may not be necessary.
However, if there are any red flags or if the diagnosis is uncertain, imaging or other tests may be ordered to ensure a thorough evaluation.
Common investigations include:
- X-ray: Useful for identifying rib fractures or significant spinal issues.
- Blood Tests: Can reveal signs of infection or systemic inflammation.
- CT Scan or MRI: Provide detailed images of soft tissues, the spine, and internal organs if a more serious condition is suspected.
Being sent for a test is not necessarily a cause for alarm. It is often a methodical step to rule out other possibilities and confirm a diagnosis. This is also the stage where treatment options are considered; for those with persistent pain, understanding how MLS Laser therapy for chronic back pain relief works can provide valuable insight into modern therapeutic approaches.
This systematic approach is standard practice. According to Arthritis UK, around 16.9% of adults in England—approximately 5.5 million people—live with some form of back pain. Many of these cases involve discomfort that is aggravated by the mechanics of breathing.
Since symptoms can overlap between the chest and back, a comprehensive understanding is helpful. Our guide to chest pain offers a structured overview that complements this information.
So, What Does This All Mean For You?
This article has covered why back pain can occur with breathing, how clinicians approach the symptom, and which signs require medical attention. Grasping these fundamentals is the first step toward feeling more in control and making informed decisions about your health.
Pain is a very common experience. In the UK, it's estimated that 43% of adults—nearly 28 million people—are living with some form of chronic pain. Back pain is a significant part of this, and due to the interconnectedness of the spine, ribs, and diaphragm, it's not surprising that breathing can be involved. You can explore more about these UK pain statistics for a broader perspective.
Looking Beyond This One Symptom
For many, understanding a single symptom is just the beginning. Learning to connect what you feel with potential causes and available options is a skill applicable to any health challenge. It is about viewing your body as an interconnected system.
This is why we have developed a library of in-depth resources.
Our goal is to offer a more structured way to learn about your health. Instead of navigating disconnected search results, our guides provide a complete, step-by-step overview of specific conditions.
We created these for people who find this level of detail helpful and want to apply the same organised approach to other health topics.
A Clearer Path to Understanding
If you wish to move beyond single articles and build a more solid foundation of knowledge, our guides are designed to support that. They provide a clear framework, helping you see the bigger picture whether you're facing a new diagnosis or supporting someone you care about.
- From Confusion to Clarity: They are structured to cut through the noise and anxiety that often accompany health-related searches.
- Deeper Explanations: Each guide goes into far more detail than a single blog post can, explaining how different aspects of a condition are linked.
- Informed Conversations: Our aim is to provide you with the confidence and vocabulary to have more productive conversations with your doctors.
For readers wanting a structured overview, our full library of patient guides is available for you to explore.
A Few Common Questions Answered
Here are clear, practical answers to some of the questions that often come up when discussing back pain linked to breathing.
Could My Poor Posture Be The Real Culprit?
Yes, it is one of the most common contributing factors. Spending hours slumped over a desk can cause the mid-back (thoracic spine) and rib cage to become stiff and compressed. This forces the small muscles between the ribs and the main breathing muscle, the diaphragm, to work harder during normal respiration.
When you take a deep breath, you are essentially stretching muscles and joints that are already overworked, which can trigger a sharp pain. Over time, this can also contribute to low-grade inflammation in the spinal joints, making them more sensitive to the movement of breathing.
Can Anxiety Make The Pain Feel Worse?
There is a strong connection between anxiety and physical pain. When you are anxious, your breathing pattern often changes unconsciously, becoming more shallow and rapid. This pattern tends to be driven by the neck and chest muscles rather than the diaphragm.
This habit can increase tension in the shoulders and upper back. Additionally, anxiety can make the brain more sensitive to pain signals. A minor muscle twinge that might otherwise go unnoticed can feel intense and alarming. This can create a cycle where pain increases anxiety, and anxiety, in turn, amplifies the sensation of pain.
Should I Be Using Heat Or Ice?
This depends on when the pain started.
If it's a new, sharp pain from an injury within the last 48 to 72 hours, an ice pack is often recommended. Ice can help reduce inflammation and numb the immediate pain. Apply it for about 15 minutes at a time.
For a persistent, chronic ache or general muscle stiffness without obvious swelling, a heat pack is usually more beneficial. Heat helps relax tight muscles and increases blood flow to the area, which can provide soothing relief.
Is It Actually Safe To Exercise When It Hurts To Breathe?
This depends entirely on the cause of the pain. If it is a mild muscle strain, gentle movement is often beneficial. A slow walk or very careful, targeted stretches can help prevent stiffness and promote blood flow, which supports healing.
However, if the pain is severe, sharp, or accompanied by any red flag symptoms (like fever or shortness of breath), you should stop and seek medical advice. Never "push through" sharp pain. A doctor or physiotherapist can provide a proper diagnosis and advise on what movements are safe and when to begin them.
At The Patients Guide, our goal is to provide structured, clear information that helps you build a deeper understanding of your health. If you found this approach helpful, you may wish to explore our full library of in-depth health guides.
Learn more at https://www.thepatientsguide.co.uk.
Also in News

A Calm Guide to Treating Whiplash at Home
February 10, 2026 10 min read
Feeling overwhelmed by neck pain after an injury? This is a calm, clear guide to treating whiplash at home, focusing on safe pain relief and recovery.
Read More
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
