Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
A Calm Guide to Treating Whiplash at Home
February 10, 2026 10 min read

Dealing with a whiplash injury can be a confusing mix of pain, stiffness, and uncertainty. If you are searching for answers, you have likely found conflicting advice online—some suggesting complete rest, others pushing for immediate movement.
This can be frustrating when all you want is a clear path forward.
The clinical approach today focuses on a careful balance: managing symptoms while encouraging gentle movement, but only within a range that feels safe. This article explains how healthcare professionals think about this process, starting with the first 72 hours.
The First 72 Hours After a Whiplash Injury

In clinical settings, the initial goal is to manage the acute symptoms without letting the neck muscles seize up. Completely stopping all movement can sometimes lead to more stiffness and a longer recovery, so the focus is on calming the injury while maintaining gentle function.
The Initial Focus: Pain and Inflammation
Immediately after the injury, your body’s inflammatory response begins. This is a normal part of healing, but it is also the source of much of the initial swelling and pain. Managing this is the first priority.
- Cold Therapy (First 24–48 hours): In the first two days, applying cold can be helpful. Wrap an ice pack or frozen peas in a thin towel and place it on the most painful areas of your neck. Aim for 15-20 minutes at a time, several times a day. This helps constrict blood vessels, which may reduce swelling and numb the sharpest pain.
- Warmth (After 48–72 hours): Once the initial, acute inflammation has settled, you can introduce warmth. A warm compress, hot water bottle, or a warm shower can help relax tense muscles. Heat increases circulation to the injured tissues, which supports the healing process.
Headaches are also commonly seen with whiplash, often caused by muscle tension that travels from the back of the neck to the base of the skull. To understand more about the connection between neck injury and head trauma symptoms, our article on Post-Concussion Syndrome provides further context.
Balancing Rest with Gentle Activity
Healthcare professionals often use the term "relative rest." This means avoiding activities that clearly strain your neck—such as heavy lifting or sudden head movements—but not lying in bed for days.
The key is to listen to your body. Gentle movement is generally beneficial, but pushing through sharp, stabbing pain is not.
Staying completely still may cause neck muscles to weaken and stiffen. This can make it much harder to regain your full range of motion later. The goal is to keep your neck moving in small, slow, controlled ways to prevent this from happening.
Even with effective self-care, recovery takes time. Research has shown that a significant number of people still experience some symptoms weeks after an injury. This highlights that while home treatment is the foundation, whiplash recovery is often a gradual process.
Managing Pain and Stiffness at Home
Once you are past the first 72 hours, your focus will likely shift to managing ongoing pain and stiffness. This phase is about finding a sustainable rhythm that keeps discomfort at a manageable level, allowing you to begin the gentle movements your neck needs.
The aim is not to eliminate all sensation. Instead, these methods can create windows of opportunity where movement feels more comfortable and less restricted.
Over-the-Counter Medication Options
For many, over-the-counter pain relief is a sensible starting point. Understanding the different types can help you use them effectively.
- Paracetamol: This is often a good first choice. It works on pain signals in the brain and can help take the edge off a general, nagging ache.
- Anti-inflammatories (NSAIDs): Medications like ibuprofen target inflammation in the injured soft tissues. They may be particularly helpful if you have persistent warmth or noticeable swelling.
It is important to follow the dosage instructions on the packet. If you have other health conditions or are taking other medications, check with a pharmacist or your GP first. The goal is to manage symptoms enough to move gently, not to mask them completely. Pain can be a useful signal to avoid overdoing it.
Using Ice and Heat Strategically
After the first few days, the use of ice and heat becomes more flexible. You can tailor your approach to what your body needs at any given moment.
As a general guideline, many clinicians suggest using heat for stiffness and ice for flare-ups of sharp pain.
For example, applying a warm compress for 15-20 minutes before you do gentle stretches can help relax tight muscles, making movement feel smoother.
On the other hand, if you have had a busy day and your neck feels sore and aggravated, an ice pack for 15 minutes can help calm down the irritation.
To clarify these common home pain relief methods, the table below provides a summary.
Home Pain Relief Methods for Whiplash
This table outlines the purpose and application of common techniques for managing whiplash pain at home during your recovery.
| Method | Primary Purpose | When to Use | Typical Application |
|---|---|---|---|
| Ice Pack | Reduce inflammation and numb acute pain. | First 48-72 hours; also for flare-ups later. | Wrap in a towel; apply for 15 minutes at a time. |
| Heat Pack | Relax muscle tightness and improve blood flow. | After the initial inflammatory phase (post-72 hours). | Use a warm compress for 15-20 minutes, especially before stretching. |
| Paracetamol | General pain relief. | For dull, aching pain throughout recovery. | Follow packet instructions; a good first-line option. |
| NSAIDs (Ibuprofen) | Reduce inflammation and relieve pain. | When inflammation is a key symptom (pain, stiffness, warmth). | Follow packet instructions; check with a pharmacist if unsure. |
Whiplash headaches, often stemming from intense neck muscle tension, are also very common. If this is a primary concern, our guide on natural remedies for tension headaches offers complementary strategies.
Reintroducing Gentle Neck Movements
It is a natural instinct to keep your neck still when it hurts, and for a long time, medical advice often involved rest and immobilisation with a neck collar.
However, clinical understanding has evolved. Evidence now suggests that gentle, controlled movement is one of the most important components of recovery. Keeping the neck completely static can cause the muscles and ligaments to tighten and weaken, which may lead to chronic stiffness.
The key is to reintroduce movement slowly, always paying close attention to your body’s signals.
Before you begin, managing the acute pain and inflammation is important. This is where the initial use of cold, warmth, and medication is helpful.
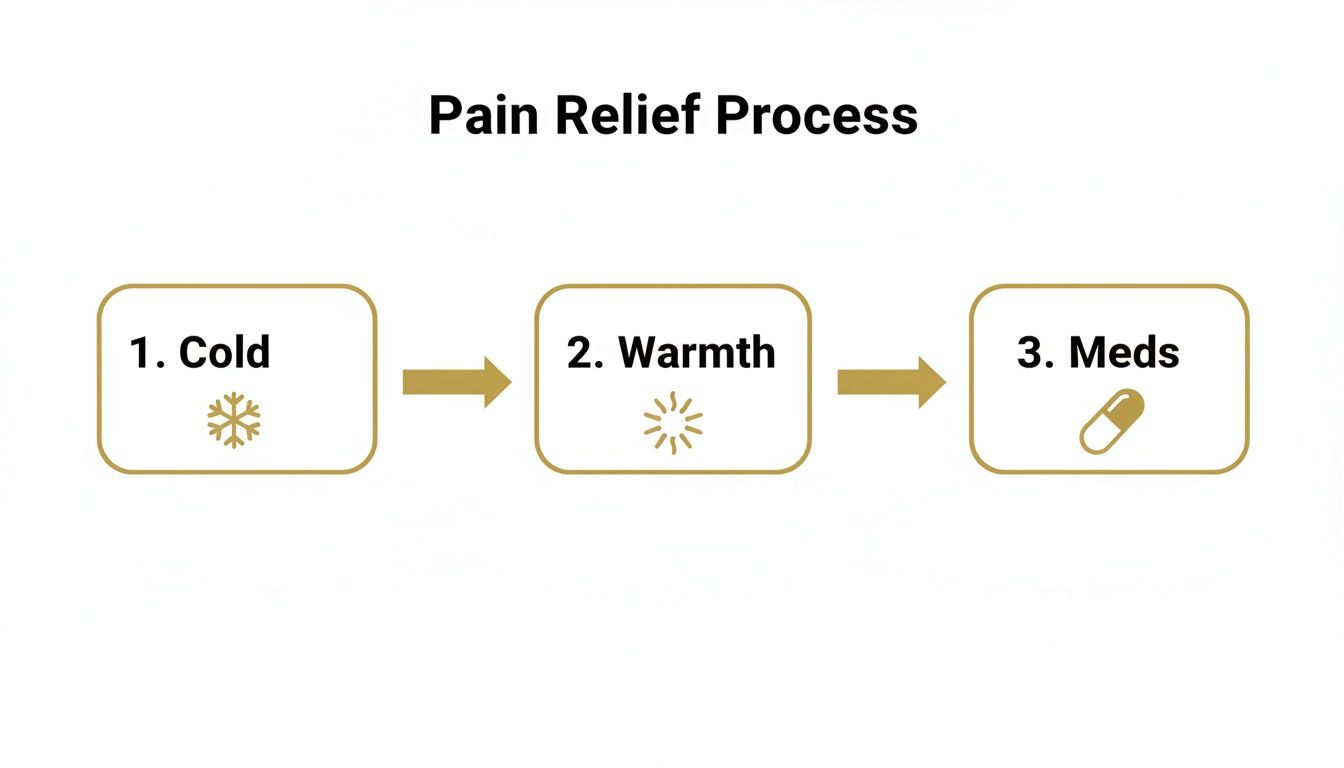
By addressing inflammation with cold, using warmth to relax muscles, and taking medication to reduce pain, you create a better window for these gentle movements to feel manageable.
Foundational Range-of-Motion Exercises
The goal here is not to push through pain, but to gently explore the movement you have available. Perform these slowly and with control. A mild stretching sensation is normal, but any sharp, stabbing, or radiating pain is a signal to stop.
- Gentle Nods (Flexion/Extension): While sitting or standing with good posture, slowly tuck your chin toward your chest. Hold for a moment, then gently return your head to the neutral starting position.
- Slow Head Turns (Rotation): Keeping your chin level, slowly turn your head to look over one shoulder. Go only as far as is comfortable. Pause, return to the center, and repeat on the other side.
- Side Tilts (Lateral Flexion): Gently tilt your ear toward your shoulder, without letting your shoulder lift up. You should feel a light stretch along the opposite side of your neck. Return to the start and repeat on the other side.
A guiding principle is to always work within a pain-free zone. Forcing movement can cause muscles to guard and may increase inflammation. You are gently reminding your neck it is safe to move.
Try performing 5-10 repetitions of each movement a few times throughout the day. Short, frequent sessions are often more effective than one long, painful one.
As the acute pain subsides, and with professional guidance, you might consider incorporating something like Pilates for rehabilitation. It can be an effective way to rebuild strength and stability in the neck and core.
As you become more comfortable, you can gradually increase the range of these movements. This patient approach helps build confidence and prevent setbacks.
Small Changes, Big Impact: Adjusting Your Daily Habits

While specific exercises are important, your activities during the rest of the day also matter. Small details in your daily life can either support or hinder the healing process.
Your neck is constantly working, from how you sit at a desk to how you sleep. When it is already injured, even minor, sustained stress can increase pain and slow down recovery.
By making a few conscious adjustments, you can reduce this background strain and create a better environment for healing.
Create a Neck-Friendly Workspace
If you work at a desk, your setup can be a source of aggravation for whiplash. Poor ergonomics can force your neck into awkward positions for hours. The goal is to achieve a neutral posture.
A few simple changes can make a significant difference:
- Monitor Height: The top of your screen should be at or slightly below eye level. This helps prevent you from slouching forward or craning your neck.
- Back Support: Use a chair with good lumbar support to help your entire spine maintain a healthy alignment. Keep your feet flat on the floor.
- Arm Position: Your elbows should be at roughly a 90-degree angle, with your wrists straight. This reduces tension in the shoulders that can travel up to your neck.
These adjustments can reduce the load on your neck muscles, allowing them to rest and recover, even while you work.
Master Your Sleep Position
Sleep is when your body does much of its repair work. An awkward sleeping position can leave you feeling worse in the morning. The goal is to keep your neck aligned with the rest of your spine.
The two best positions are generally on your back or your side. Sleeping on your stomach should be avoided, as it forces your head to twist for long periods, straining the neck.
If you sleep on your back, a single, lower pillow that supports the natural curve of your neck is often best. For side sleepers, a slightly firmer or thicker pillow may be needed to fill the space between your ear and the mattress, keeping your head level.
Keep Moving, Gently
While strenuous activity should be avoided, complete rest is also not the answer. Light activity, like walking, is beneficial. It improves blood flow, delivering oxygen and nutrients to injured tissues.
It also prevents muscles from becoming weak and stiff from inactivity. This active approach is supported by evidence; you can read about the NHS approach in this factsheet on whiplash.
By integrating these habits into your day, you create a recovery-focused environment that supports your body’s natural healing process.
When to See a Professional
While most whiplash injuries can be managed at home, it is important to recognise the limits of self-care. Knowing when to continue your routine and when to seek a professional opinion is a key part of a safe recovery.
Healthcare professionals look for specific signs, sometimes called ‘red flags’, that might indicate a more serious issue. If you notice any of the following, it is wise to consult your GP or visit an urgent care centre.
Red Flag Symptoms to Watch For
Seek a professional medical opinion if you experience any of the following, as they could suggest something more than a straightforward soft tissue injury.
- Severe or worsening headaches: While a mild headache is common, a headache that comes on suddenly, feels severe, or gets progressively worse requires attention.
- Dizziness or balance issues: Feeling unsteady or experiencing a spinning sensation (vertigo) should be evaluated by a professional.
- Weakness or numbness: Any new weakness, significant numbness, or a persistent "pins-and-needles" sensation in your arms or hands needs to be assessed.
- Changes in vision or hearing: This includes blurred vision, double vision, or a constant ringing in your ears (tinnitus).
It is also important to recognise if your recovery seems to have stalled. Home treatment should lead to slow but steady improvement.
Signs Your Recovery Has Stalled
Consider consulting your GP or a physiotherapist if you notice these patterns:
- Your pain has not started to ease after a week of consistent self-care, or if it is getting worse.
- Your neck's range of motion is not improving after a week or two of gentle exercises. A physiotherapist can help create a more targeted plan.
Sometimes, symptoms that seem like whiplash can involve other issues, such as nerve irritation. You can learn more about related conditions in our article on Cervical Radiculopathy.
It may be reassuring to know that most people recover well at home. A UK study found that while many patients visited their GP, positive outcomes were often linked to consistent self-care, like using painkillers and doing gentle exercises. You can read the full research about these findings for more detail.
Knowing these guidelines can help you manage your recovery responsibly, providing clarity on when to seek professional support.
Common Questions About Whiplash Recovery
It is normal to have questions when managing a whiplash injury. Understanding what to expect can help you feel more in control of the healing process. Here are some of the most common queries.
Should I Use a Neck Collar for Whiplash?
The advice on neck collars has changed significantly over the years. For most cases of whiplash, soft collars are no longer recommended. While the previous approach emphasised immobilisation, we now understand that keeping the neck still for too long can lead to increased stiffness and weaker muscles.
The current focus is on encouraging gentle, early movement to maintain flexibility. A collar might be used for a very brief period in severe cases under direct medical supervision, but for most people, it is best avoided.
How Long Does Whiplash Recovery Take?
There is no single answer to this question, as recovery varies from person to person. Many people feel significantly better within a few weeks, and most recover within two to three months with a consistent home care plan.
For some, however, symptoms can linger. An overview of the typical whiplash injury recovery time can provide a clearer picture of the timelines. The focus should be on steady, gradual progress rather than a specific end date.
Recovery is rarely a straight line; there will be good days and bad days. The important thing is that the overall trend is toward improvement.
Can I Go to Work with Whiplash?
For many people, continuing to work is encouraged. Maintaining a normal routine can be beneficial for both physical and mental well-being, provided that sensible adjustments are made.
This may mean avoiding tasks that involve heavy lifting or sitting in one position for long periods. Discussing simple ergonomic changes to your workstation with your employer can also be very helpful. Unless your symptoms are severe or your job places direct strain on your neck, prolonged absence from work is not usually recommended.
When Is It Safe to Drive Again?
Safety must be the priority. You should only return to driving when you can comfortably turn your head to check blind spots and react quickly without a sharp increase in pain.
Before driving, sit in the car and practice the necessary movements. Can you look over your shoulder without significant pain? Can you check your mirrors easily? If you are taking any pain medication that could cause drowsiness, you must not drive. If you are in doubt, consult your GP.
We hope this article has helped reduce confusion and provide a clear framework for managing whiplash at home. We also recognise that online articles have their limits.
For those wanting a structured overview that goes into greater depth, The Patients Guide offers more detailed resources. Our guides are designed to connect concepts, explain recovery patterns, and support long-term understanding so you can make informed decisions.
To explore our full library of guides, you can visit us at https://www.thepatientsguide.co.uk.
Also in News
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Understanding Your LFT Blood Test: A Patient's Guide
February 07, 2026 11 min read
Confused by your LFT blood test results? This clear guide explains what the markers mean, how doctors interpret them, and what to expect next.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
