Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
Understanding Abdominal Pain After Eating
February 02, 2026 13 min read
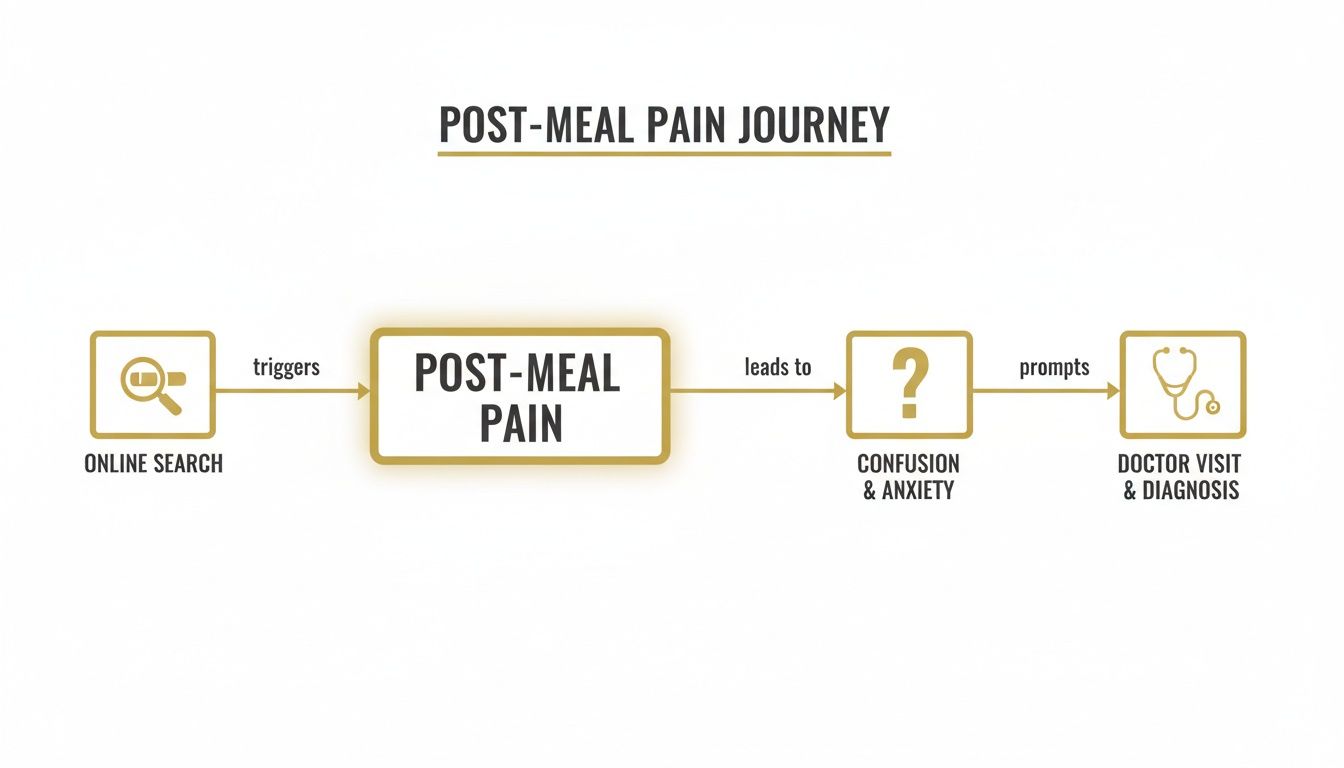
Experiencing abdominal pain after a meal is a common and often frustrating problem. Searching for answers online can be confusing, with one source suggesting simple indigestion and another pointing to something more serious. This conflicting information often leads to more anxiety, not less.
This guide is designed to provide clarity. It is not a diagnostic tool or a list of quick fixes. Instead, the goal is to explain how healthcare professionals typically think about and investigate abdominal pain that occurs after eating.
Living with this kind of discomfort can be draining. The uncertainty about what might trigger the pain can affect your relationship with food and your social life.
We will walk through the common patterns and potential causes that clinicians consider, step by step. The aim is to replace confusion with a clearer understanding, helping you feel better equipped to interpret what your body might be telling you.
By understanding the framework used in clinical settings, you can move from a state of uncertainty to one of informed awareness. This shift is often the first step towards feeling more in control of your health.
To help build this understanding, we will cover several key areas:
- Common Causes: We will explore the most frequent reasons for post-meal pain, from functional issues like indigestion and IBS to specific food intolerances.
- The Clinical Investigation: You’ll learn about the questions a doctor may ask and the examinations they might perform to understand the underlying cause.
- Practical Steps at Home: We’ll cover sensible, evidence-based steps you can take to start identifying your triggers and managing symptoms.
This information is intended to support, not replace, a consultation with a healthcare professional. For readers who want to explore their digestive health in more detail, we have developed a library of resources. You can browse our collection of abdominal patient guides for more structured information on specific conditions.
By the end of this article, you should have a clearer framework for navigating your symptoms and feel better prepared for a productive conversation with your doctor.
Common Causes of Pain After Eating
Many people describe a familiar pattern: a nagging or sharp pain begins after a meal, leading to online searches that often create more questions than answers. This experience highlights the importance of professional guidance in finding clarity.
Let's look at some of the most common reasons a clinician would consider when investigating abdominal pain that occurs after meals.
Functional Digestive Issues
In many cases, the pain is not caused by a structural problem with the digestive organs, but rather by how they function. These are known as functional digestive issues, meaning that while the system may appear normal on scans, it isn't working optimally.
A common example is Indigestion (Dyspepsia). This is not a single disease but a term for symptoms like upper abdominal pain, bloating, or a premature feeling of fullness. It often suggests the stomach is having difficulty processing and moving food efficiently.
Irritable Bowel Syndrome (IBS) is another common functional disorder. In people with IBS, the gut can be hypersensitive. The normal stretching and contracting that occurs during digestion may be perceived as painful, leading to cramping, bloating, gas, and changes in bowel habits.
Food Intolerances and Sensitivities
Sometimes, the cause is a specific ingredient that the body struggles to process, leading to a direct reaction in the gut. It is important to distinguish these intolerances, which are digestive issues, from true allergies, which involve an immune system response.
Common examples include:
- Lactose Intolerance: This occurs when the body lacks the enzyme to properly digest the sugar in milk and dairy products. This can result in gas, bloating, and crampy pain, typically within a few hours of consumption.
- Gluten Sensitivity: For some individuals without coeliac disease, gluten (a protein in wheat, barley, and rye) can trigger significant digestive upset, including pain and bloating.
Another potential issue is what is fructose intolerance, where the body has difficulty absorbing this particular sugar. Identifying these triggers usually requires careful observation of diet and symptoms.
Structural or Inflammatory Conditions
Pain after eating can also be a sign of a structural problem or inflammation within a digestive organ. While less common than functional disorders, a clinical assessment is needed to rule them out.
Gallbladder Problems: The gallbladder releases bile to help break down fats. If gallstones form and cause a blockage, this can lead to sudden, sharp pain in the upper right abdomen, particularly after a fatty meal.
Gastritis: This is inflammation of the stomach lining. It can be caused by infections (like H. pylori), long-term use of certain medications (e.g., anti-inflammatories), or excessive alcohol intake. The pain is often described as a gnawing or burning sensation.
Pancreatitis: Inflammation of the pancreas can cause a severe, persistent pain in the upper abdomen that may radiate to the back. This pain often worsens after eating and can be a medical emergency.
To provide a clearer overview, the following table summarises some common causes.
Common Causes of Post-Meal Abdominal Pain at a Glance
This table outlines frequent causes of pain after eating, along with typical symptoms and timing. It can be used to help identify patterns, but it is not a substitute for a professional diagnosis.
| Cause | Common Symptoms | Typical Onset After Eating | Pain Character |
|---|---|---|---|
| Indigestion | Upper abdominal pain, bloating, early fullness | Shortly after eating | Gnawing, burning, discomfort |
| IBS | Cramping, bloating, gas, diarrhoea/constipation | Can be immediate or delayed | Spasmodic, cramp-like |
| Lactose Intolerance | Bloating, gas, diarrhoea, cramps | 30 minutes to 2 hours | Crampy, gassy pain |
| Gallstones | Sudden, intense pain in upper right abdomen | Often after a fatty meal | Sharp, severe, constant |
| Gastritis | Burning or gnawing pain in upper abdomen | Can worsen with eating | Burning, aching |
Paying attention to when the pain begins and what it feels like can provide your doctor with valuable information.
Experiencing this is remarkably common. A 2016 YouGov survey in the UK found that of the 43% of the population who had experienced digestive issues, 63% identified abdominal pain as their most frequent symptom.
How a Doctor Investigates Your Symptoms
When you consult a GP about abdominal pain after eating, their approach is methodical. They act like a detective, gathering clues to understand the situation, rule out serious conditions, and identify the likely cause. Understanding their thought process can make the experience less intimidating.
The investigation almost always begins with a detailed conversation. This is often the most critical part of the assessment, as the history of your symptoms provides the framework for all subsequent steps.
The Medical History: A Crucial First Step
Your doctor will ask a series of specific questions to build a clear picture of your experience. Each question helps narrow the field of possibilities.
They will typically focus on a few key areas:
- Location: Where exactly is the pain? Is it in the upper right quadrant (which might suggest the gallbladder), central (often stomach-related), or in the lower abdomen (which could indicate the intestines)?
- Timing: How soon after eating does the pain start? Immediate pain may point to the stomach, while pain that develops an hour or two later could be related to the small intestine or gallbladder.
- Quality: What does the pain feel like? Is it sharp, dull, burning, or cramping? Your description provides important clues.
- Triggers and Relief: Are there specific foods, like fatty or spicy meals, that consistently trigger it? Does anything provide relief, such as passing wind or having a bowel movement?
This conversation helps the clinician form a working hypothesis, much like a detective gathering witness statements.
The Physical Examination
Following the medical history, a physical examination adds another layer of information. The doctor will gently press on different areas of your abdomen to check for tenderness, swelling, or unusual firmness.
They are looking for specific signs:
- Localised Tenderness: Pain in a specific spot can help pinpoint the affected organ. For example, sharp pain in the lower right abdomen might raise concerns about appendicitis, which can sometimes be aggravated by digestive changes. You can learn more in our detailed guide on understanding appendicitis.
- Guarding: This is an involuntary tensing of the abdominal muscles, a protective reflex that often indicates underlying inflammation.
- Bowel Sounds: Using a stethoscope, a doctor can listen to the sounds of your digestive system. Whether they are unusually active or quiet can provide valuable information.
This hands-on assessment helps to support or challenge the initial ideas formed during your conversation.
In a clinical setting, the combination of a detailed patient history and a thorough physical exam provides enough information to form a likely diagnosis in a significant number of cases. Diagnostic tests are often used to confirm these findings, not to search for a problem blindly.
Identifying "Red Flag" Symptoms
Throughout the consultation, your doctor will also be watchful for "red flag" symptoms. These are signs that may suggest a more serious condition, prompting a more urgent or in-depth investigation.
Key red flags include:
- Unexplained Weight Loss: Losing weight without trying can be a sign that the body isn't absorbing nutrients properly.
- Blood in Your Stool: This should always be investigated by a medical professional.
- Difficulty Swallowing: Known as dysphagia, this can indicate a problem with the oesophagus.
- Persistent Vomiting: This is especially concerning if it contains blood.
- Fever and Chills: These often signal an infection or significant inflammation.
If you have one or more of these symptoms, your doctor will likely recommend further tests, such as blood work, stool samples, or imaging like an ultrasound or endoscopy, to get a clearer picture.
The Link Between IBS and Meal-Related Pain
If you experience persistent abdominal pain after eating and other physical causes have been ruled out, Irritable Bowel Syndrome (IBS) is often a primary consideration. IBS is not a condition of visible damage or inflammation; instead, it's understood as a disorder of gut-brain interaction.
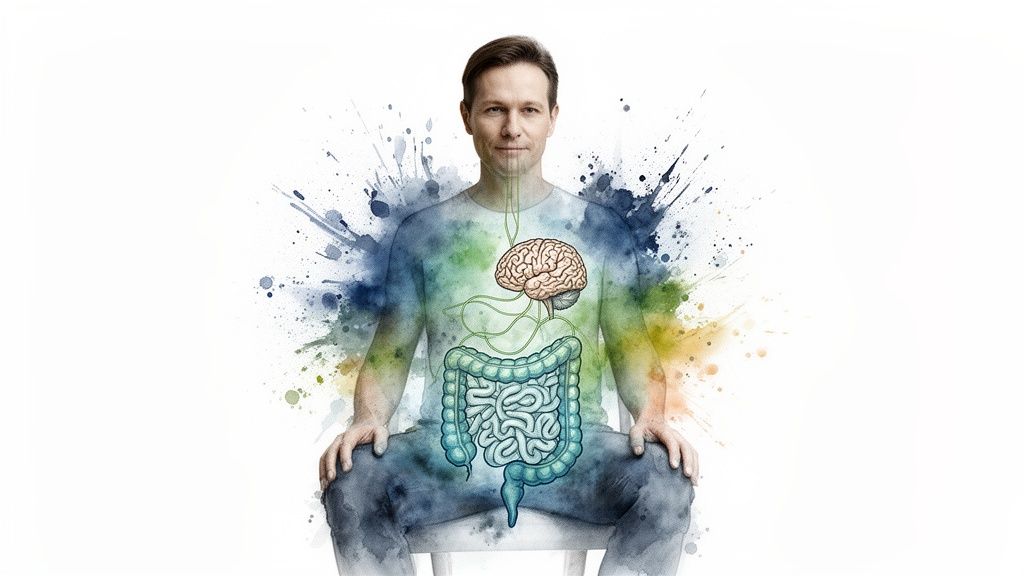
In simple terms, IBS involves a communication issue between the gut and the brain. This can trigger very real, physical symptoms, with pain after meals being one of the most common.
Understanding the Gut-Brain Axis
The connection between your gut and brain is a busy, two-way communication pathway known as the gut-brain axis. Nerves and chemical messengers constantly travel between the two, influencing both digestion and emotional states. In IBS, this communication network can become disrupted.
The gut contains its own complex nervous system, sometimes called the "second brain." If this system becomes overly sensitive, even normal digestive processes—like the stomach stretching to accommodate food—can be interpreted by the brain as a threat, triggering a pain response.
The Role of Visceral Hypersensitivity
A key concept in understanding IBS is visceral hypersensitivity. This term simply means having an overly sensitive gut. The nerves in the digestive tract are on high alert and have a lower pain threshold than usual.
For someone with visceral hypersensitivity, normal digestive sensations, like gas moving through the intestines, can trigger an intense pain response. This is why a standard meal can cause significant discomfort for a person with IBS, while someone else might feel nothing.
This heightened sensitivity explains why pain after eating is a hallmark of the condition. Managing IBS often involves strategies to calm this hypersensitivity, including diet, stress management, and sometimes medication. Exploring options like probiotics and gut health supplements can also play a supportive role in an overall management plan.
Post-meal abdominal pain is frequently associated with irritable bowel syndrome (IBS). The British Journal of Medical Practitioners estimates the prevalence of IBS in the UK at 17% overall, with higher rates in women (20-25%) compared to men (11%). Learn more about the impact of IBS from this research.
FODMAPs as a Common Trigger
Diet is a cornerstone of managing IBS, and one of the most studied approaches involves understanding FODMAPs. This acronym stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
These are specific types of short-chain carbohydrates that the small intestine can have trouble absorbing. When these undigested carbohydrates reach the large intestine, they can cause two main problems for people with IBS:
- They draw extra water into the bowel, which may lead to diarrhoea.
- They are rapidly fermented by gut bacteria, producing excess gas that causes bloating, cramping, and pain.
Common high-FODMAP foods include wheat, onions, garlic, certain fruits like apples, and many dairy products. A low-FODMAP diet, which should be undertaken with professional guidance, involves temporarily restricting these foods and then systematically reintroducing them to identify personal triggers. It is not a lifelong diet but a diagnostic tool for creating a sustainable, personalised eating plan.
Practical Steps for Managing Symptoms at Home
While awaiting a formal diagnosis or medical guidance, there are practical steps you can take. This is not about restrictive dieting but about becoming more aware of your body's patterns and making thoughtful adjustments.

The goal is to build sustainable habits to better understand your triggers and potentially reduce the frequency and intensity of abdominal pain after eating.
The Value of a Food and Symptom Diary
One of the most effective tools is a simple food and symptom diary. For one to two weeks, keep a record of everything you eat and drink, noting the time of consumption. Crucially, also log any symptoms you experience, their intensity, and when they occur in relation to your meals.
This is a data-collection exercise, not a judgment of your food choices. Over time, patterns that were not previously obvious may emerge. This information can be incredibly valuable for both you and your doctor.
Gentle Dietary Adjustments
Before considering eliminating entire food groups, some basic habits can make a significant difference in how your gut responds to food.
- Eat Smaller, More Frequent Meals: Large meals can stretch the stomach and require a significant digestive effort, which can be a trigger for pain. Try having five or six smaller meals throughout the day to keep your digestive system working steadily without being overwhelmed.
- Chew Your Food Thoroughly: Digestion begins in the mouth. Chewing food well reduces the workload on your stomach, which can lead to less discomfort after eating.
- Practise Mindful Eating: Eating while stressed or distracted can interfere with digestion. Taking the time to sit in a calm environment and eat slowly can have a surprisingly positive effect.
A core principle in managing digestive symptoms is to reduce the overall load on the system. Simple adjustments to meal size, pacing, and chewing are often more impactful than complex dietary changes, especially in the early stages of investigation.
The Influence of Lifestyle
The gut is intricately connected to your overall lifestyle, particularly stress levels and physical activity.
Stress is a known trigger for digestive issues. Due to the gut-brain axis, emotional stress can manifest as physical symptoms, including pain and increased gut sensitivity. Integrating stress-management techniques into your day can be beneficial. This might include a short 10-minute walk, deep breathing exercises, or mindfulness practices.
Similarly, gentle exercise like walking or yoga can support healthy digestion by encouraging the natural movement of the intestines, which helps prevent uncomfortable gas and bloating. For a deeper look at long-term strategies, you can explore ways to improve gut health naturally.
Taking these practical steps provides a solid framework for understanding and managing your symptoms, putting you in a more active role in your health journey. For those interested in a more structured look at dietary strategies, this topic is explored in greater detail in our comprehensive Nutrition Guides.
How Chronic Digestive Pain Affects Emotional Well-being
Living with persistent abdominal pain after eating is more than a physical issue. It can significantly impact your emotional state, changing how you view food, navigate social situations, and feel day-to-day.
There is a powerful connection between the gut and the brain, often referred to as the gut-brain axis. This means that stress and anxiety can directly affect digestion, potentially making the gut more sensitive and prone to symptoms.
The Fear-Pain Cycle
It is understandable that if eating frequently leads to pain, you might begin to feel anxious about meals. This can create a difficult cycle.
Worrying about an upcoming meal can put your digestive system on high alert. Stress hormones can increase gut sensitivity, making normal digestion feel painful. This can create a feedback loop where the fear of pain contributes to the pain itself.
In clinical practice, the emotional burden of chronic digestive problems is often as significant as the physical symptoms. Acknowledging this connection is an important step, as strategies that calm the mind can have a direct, soothing effect on the gut.
The Gut-Brain Connection in Daily Life
This link is grounded in biology. The gut is lined with an extensive network of nerves—our "second brain"—which is in constant communication with the brain. When the gut is irritated, it can send signals that directly impact mood.
Conversely, when you are stressed or anxious, the brain sends signals to the gut that can alter its motility, increase inflammation, and disrupt the balance of gut bacteria. This is why symptoms may feel worse during a stressful period, even with no changes to your diet.
Research highlights this connection. A global survey by the Rome Foundation found that among people with frequent meal-related pain, 36% also experienced anxiety and 35% reported depression, rates significantly higher than in those with only occasional pain. You can read more about these findings on meal-related pain and mood.
Understanding this relationship can be empowering. It validates the experience of feeling anxious or low due to gut symptoms and points toward helpful approaches like mindfulness or cognitive behavioural therapy, which address both mind and body to help break the cycle.
Frequently Asked Questions
Here are answers to some of the most common questions about abdominal pain after eating.
When should I see a doctor for abdominal pain after eating?
It is advisable to see a GP if the pain is severe, persistent, or recurrent. You should seek medical advice promptly if the pain is accompanied by any "red flag" symptoms, such as unexplained weight loss, persistent vomiting, blood in your stool, fever, or difficulty swallowing.
While many causes are not serious, it is important to rule out other conditions. A professional diagnosis is the only way to gain peace of mind and determine the appropriate path forward.
Can stress make my abdominal pain worse?
Yes, stress can significantly impact digestive symptoms. The gut-brain axis is a powerful two-way communication system. When you are stressed or anxious, your gut can become more sensitive, and its normal rhythm can be disrupted.
Learning to manage stress through techniques like mindfulness, gentle exercise, or simple breathing exercises can make a noticeable difference for many people. Addressing the emotional component is often a key part of managing the physical discomfort.
Is it better to eat small meals or three large ones?
For many people dealing with pain after eating, smaller, more frequent meals are often beneficial. A large meal can stretch the stomach and place a significant demand on the digestive system, which can trigger pain, bloating, and discomfort.
Spacing out smaller meals puts less strain on your digestive system, allowing it to process food more gently and effectively.
It can be helpful to experiment and use a food and symptom diary to see what works best for you. There is no single rule that fits everyone, so listening to your body is essential.
Navigating health concerns online can be overwhelming. The goal of this article was to provide a clear, grounded explanation of post-meal abdominal pain, framed by how clinicians approach the problem. Understanding the "why" behind your symptoms is the foundation for making informed decisions about your health.
For those who want a structured path forward, we created The Patients Guide. Our digital guides offer step-by-step clarity on specific conditions, helping you connect symptoms, causes, and management strategies in one organised resource.
You can explore our full library of patient-first health guides at https://www.thepatientsguide.co.uk.
Also in News
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Understanding Your LFT Blood Test: A Patient's Guide
February 07, 2026 11 min read
Confused by your LFT blood test results? This clear guide explains what the markers mean, how doctors interpret them, and what to expect next.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
