Modern healthcare is fragmented. Understanding helps connect the dots.
Modern healthcare is fragmented. Understanding helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
What Is Post Concussion Syndrome A Clear Guide to Symptoms and Recovery
January 21, 2026 13 min read
Searching for answers about a concussion that won’t go away can be frustrating. You may have been told to rest, only to find that symptoms like headaches, dizziness, and brain fog are still present weeks or months later.
Online advice often conflicts, leaving you unsure of what to believe or what to do next. This guide is designed to provide clarity. It's not about miracle claims or quick fixes.
Instead, it explains how healthcare professionals understand Post-Concussion Syndrome (PCS)—the term for symptoms that persist beyond the typical recovery window.
Our goal is to help you move from a place of uncertainty to one of informed understanding, which is the foundation for effective action.

When Symptoms Linger After a Concussion
A concussion is expected to be a short-term issue for most people. However, for a significant number, the initial symptoms become persistent, creating real challenges in daily life.
If you're still struggling to keep up with work, family life, or just feeling like your old self, you are not alone. The path can feel isolating, cluttered with contradictory advice and a nagging sense of uncertainty.
This article aims to cut through that noise by explaining the mechanisms behind persistent symptoms and the factors that can influence recovery.
Defining Post-Concussion Syndrome
To understand what PCS is—and what it isn't—this table breaks down the core concepts from a clinical perspective.
| Post Concussion Syndrome at a Glance | |
|---|---|
| Concept | Brief Explanation |
| What It Is | A complex disorder where symptoms from a mild traumatic brain injury (mTBI), or concussion, persist beyond the expected recovery window (often several weeks). |
| The Cause | Not typically due to ongoing structural brain damage. It is often a functional disruption—a problem with how the brain’s systems (like vision, balance, and autonomic control) communicate and work together. |
| Why Scans Are Often Normal | Standard imaging like MRIs and CT scans look for structural issues (such as a bleed). Since PCS is a functional problem, these scans commonly come back clear. This can be confusing, but it does not mean your symptoms aren't real. |
| Is It Common? | Having some lingering symptoms is more common than many people think. A significant number of individuals report at least one ongoing symptom months after their injury. |
Understanding these points is crucial because it shifts the focus from "Is my brain still damaged?" to "How can my brain's systems be encouraged to work properly again?"
How Common Is a Prolonged Recovery?
While it might feel isolating, a delayed recovery is far from rare. In the UK, mild traumatic brain injuries account for about 1.2% of all A&E visits. This figure may be an underestimate, as some studies have shown that hospital coding for concussions can be inaccurate in up to 90% of cases.
So, how many people experience long-term symptoms? One major UK study offered some insight: 82% of patients with an mTBI still reported at least one ongoing symptom six and twelve months after their injury. You can review the full research on concussion outcomes.
This data makes it clear: if you’re still feeling the effects of a concussion, your experience is not unusual. The next step is understanding what is happening. For a review of the crucial first steps, see our guide on what to do immediately after a concussion.
Recognising Common Symptom Patterns
Understanding Post-Concussion Syndrome often starts with seeing it not as one thing, but as a collection of issues that tend to appear in predictable groups, or ‘symptom clusters’. Organising symptoms into three main categories can provide a clearer way to make sense of your experience, rather than looking at a long, overwhelming list.
It's also important to recognise that these symptoms often interact. Poor sleep can worsen headaches, and cognitive struggles can understandably lead to frustration and anxiety. Identifying these connections is a key step toward managing them.
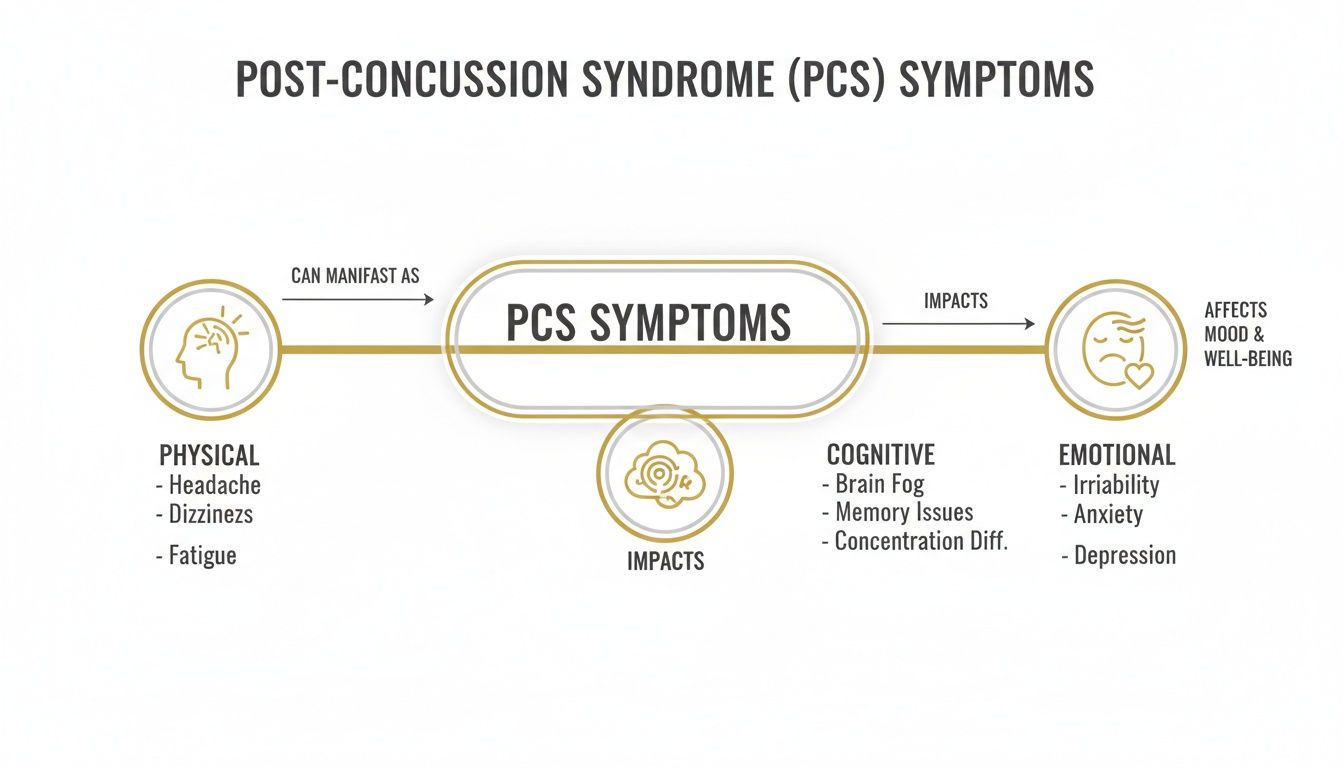
Physical Symptoms
This is the cluster most people notice first. While a range of physical symptoms can occur after a concussion, a few are especially common.
- Persistent Headaches: These are often different from typical tension headaches. They may present like a migraine, with sensitivity to light and sound, or as a relentless, dull pressure. This topic is explored in more detail in our Migraine Guide.
- Dizziness and Balance Issues: You might feel unsteady, light-headed, or experience vertigo, where it feels like the room is spinning. These sensations often suggest that the injury has affected your vestibular system—the brain’s control centre for balance.
- Fatigue: This isn't just feeling tired. PCS fatigue is often a deep, overwhelming exhaustion of body and mind that a full night’s sleep may not resolve.
- Sleep Disturbances: Difficulty falling asleep, waking frequently, or never feeling rested are classic signs. Poor sleep can then amplify every other symptom.
Cognitive Symptoms
This group of symptoms is often referred to as ‘brain fog’. It's a useful term, but let's break down what it can feel like day-to-day.
These cognitive issues do not mean a loss of intelligence. It often means your brain has to work much harder to perform tasks that used to be effortless.
In clinical settings, we often explain it like this: the brain is trying to run a marathon when it only expected a short walk. The energy required for simple cognitive tasks, like reading an email or following a conversation, can become immense.
Common cognitive patterns include:
- Difficulty with Concentration: Finding it hard to focus, getting easily distracted, or losing your train of thought mid-sentence.
- Memory Problems: This usually affects short-term memory. You might forget recent conversations or struggle to recall why you entered a room.
- Slower Processing Speed: It can feel as though your brain is lagging, taking longer to absorb information or formulate a reply.
Emotional and Mood-Related Symptoms
The impact of a persistent injury on your emotional state is real and a core part of the PCS picture. These changes are not a sign of weakness; they are often a direct result of the brain injury, compounded by the stress of coping with other symptoms.
You might find yourself becoming easily irritated, tearful, or experiencing new levels of anxiety or low mood. Often, these feelings are tied to the frustration of not being able to think, feel, and act as you once did.
Post-concussion syndrome is common in the UK. Some studies have found that among people with ongoing symptoms after a head injury, the rate is as high as 47.8%. You can explore the data behind this in our comprehensive guide references.
Understanding Why Symptoms Persist
One of the most difficult questions after a head injury is, "Why do I still feel this way?" The answer is rarely about a single part of the brain that hasn't healed. Instead, persistent symptoms are now understood to be related to a disruption of the body's core operating systems.
The initial impact can throw the delicate communication networks that manage everything from balance to heart rate out of sync.
Think of it less like a broken bone and more like a software glitch. The hardware may be fine, but the programs are not communicating correctly. This helps explain why symptoms can feel so varied and unpredictable.
When Your Body's Key Systems Are Disrupted
A few critical systems are commonly affected after a concussion. Understanding their function sheds light on why symptoms can linger.
- The Autonomic Nervous System (ANS): This is your body's "automatic" control centre, managing heart rate, blood pressure, and digestion. A concussion can disrupt the ANS, leading to a racing heart when you stand up, dizziness, and profound fatigue. The body can get stuck in an inefficient mode, unable to match its energy supply to demand.
- The Vestibular and Ocular Systems: Your sense of balance and your vision work as a team. The vestibular system in your inner ear tells your brain where your head is, while your eyes confirm it. When a concussion disrupts the signals between them, you can experience dizziness, motion sensitivity, and trouble focusing. This mismatch helps explain why a busy supermarket can feel so overwhelming.
The Role of Blood Flow and Inflammation
Beyond these system-wide disruptions, two other factors are often at play.
Cerebral Blood Flow Regulation
A healthy brain directs blood flow to the areas that are working hardest. After a concussion, this vital process, known as neurovascular coupling, can be impaired.
When the brain can't get enough oxygen-rich blood to its active cells, it can trigger an "energy crisis." This is a significant reason why even minimal mental or physical effort can bring on headaches and brain fog.
Healthcare professionals often see this mismatch between energy demand and supply as a core driver of post-concussion symptoms. The goal of rehabilitation is not to "push through," but to gently guide this system back to functioning efficiently.
Persistent Inflammation
The initial injury triggers an inflammatory response, which is a normal part of healing. In some individuals, this low-level neuroinflammation may not switch off as it should. This can disrupt brain cell function, contributing to a general feeling of being unwell, fatigued, and foggy.
Why Pre-Injury Health Matters
It is also important to recognise that your health before the injury can play a role in recovery. Certain pre-existing conditions can make the nervous system more vulnerable.
- A history of migraines: If you are prone to migraines, your nervous system may already be more sensitive. A concussion can lower your trigger threshold, leading to more frequent or intense headaches.
- Anxiety or depression: Pre-existing mood conditions can complicate recovery. The body's stress-response systems might already be on high alert, making it harder for the nervous system to rebalance after an injury.
- Previous concussions: Each concussion can make the brain more susceptible to the next and may prolong recovery time.
Understanding these interconnected factors explains why a comprehensive treatment approach is often necessary. Treating one symptom in isolation, like headaches, while ignoring an underlying balance issue, tends to be less effective.
How Professionals Diagnose and Evaluate PCS
Receiving a clear diagnosis can be a significant step forward. It validates your experience and helps establish a path to recovery. However, there is no single scan or blood test for Post-Concussion Syndrome.
Unlike a broken bone visible on an X-ray, PCS is what is known as a diagnosis of exclusion. A clinician's first job is to rule out other potential medical reasons for your symptoms. Then, they look for a specific pattern of issues that points toward a prolonged concussion recovery.
The process is a detailed investigation, pieced together from a comprehensive clinical assessment.
The Foundation: A Thorough History
The most important part of the evaluation is the clinical interview. A skilled healthcare professional will aim to understand the complete picture of your experience.
They will likely ask about:
- The Injury Itself: The specifics of the incident are important, even if it seemed minor.
- Symptom Timeline: When symptoms started, how they have changed, and what your main triggers are.
- Pre-existing Health: Your medical history provides crucial context. A past record of migraines, anxiety, or previous head injuries helps connect the dots.
This detailed conversation allows the clinician to create a map of your symptoms and how they may be linked.
The Neurological and Physical Examination
After discussing your history, the clinician will conduct a hands-on physical exam. This is designed to identify subtle problems with how your body is functioning.
The exam often includes tests to check your:
- Cranial Nerves: Simple but informative tests for vision, hearing, and facial movement.
- Balance and Gait: You might be asked to walk heel-to-toe or stand with your eyes closed.
- Coordination: Simple tasks, like the finger-to-nose test, can reveal issues with motor control.
- Neck Function: The neck is often affected during a head injury. Lingering neck problems can cause headaches and dizziness that mimic PCS symptoms, so it’s vital to assess this area.
Specialised Assessments for Specific Systems
Depending on your main symptoms, you might be referred for more specialised testing to pinpoint which of your body’s systems are struggling the most.
This multi-faceted approach moves beyond a general "concussion" label to identify specific dysfunctions—like vestibular or visual problems—that need targeted rehabilitation.
Common specialised evaluations include:
- Vestibular and Ocular Motor Screening: This tests how well your inner ear's balance system and your eyes are working together. A disconnect here is a major cause of dizziness.
- Neuropsychological Testing: If you’re dealing with significant "brain fog" or memory issues, this formal testing provides objective data on cognitive function, such as attention and processing speed.
- Imaging (When Necessary): An MRI or CT scan may be used to rule out other problems, such as a bleed or structural injury. For PCS, a normal brain scan is the expected result.
This careful, step-by-step process helps ensure your diagnosis is accurate and that your treatment plan is built on a solid foundation. Emergency department data from England and Wales shows that while mild traumatic brain injury (mTBI) represents 1.2% of A&E visits, it accounts for 68% of major trauma hospital admissions. This highlights why detailed follow-up is so important. To understand the scale of this issue, you can learn more about these key UK findings.
Finding Your Way Through Evidence-Based Treatment

Once you have a clear diagnosis, the mindset can shift from passively waiting to actively managing recovery. Effective treatment for post-concussion syndrome is rarely about a single intervention. Instead, it involves a targeted rehabilitation plan for the specific systems that have been disrupted.
This often means involving a team of specialists. The goal is to gently guide these systems back toward normal function, not to push through the pain.
Matching Therapies to Your Specific Symptoms
A one-size-fits-all approach is unlikely to be effective for PCS. The key is to identify what is driving your symptoms and then match specialised therapies to those root causes.
Common PCS Symptoms and Corresponding Therapies
The table below shows how a modern, evidence-based plan targets the precise functional issues identified during an evaluation.
| Symptom Cluster | Primary Therapy Approach | What It Addresses |
|---|---|---|
| Dizziness, Vertigo, and Motion Sensitivity | Vestibular Rehabilitation | A specialised form of physiotherapy using head, eye, and body movements to retrain the brain's balance system, helping to calm dizziness and improve stability. |
| Visual Issues (Blurriness, Eye Strain) | Vision Therapy (Neuro-Optometry) | Involves exercises designed to improve how the eyes and brain coordinate. This can help with focus, tracking, and reducing visual overload in busy environments. |
| Headaches, Neck Pain, and Stiffness | Specialised Physical Therapy | This focuses on structures in the upper neck (cervical spine), which are often injured along with the head. Gentle manual therapy and specific exercises can reduce headache frequency. |
This tailored approach tends to be far more effective than trying generic treatments.
Sub-Symptom Threshold Activity
One of the most important principles in modern concussion care is sub-symptom threshold activity. This represents a shift away from the outdated advice of total rest.
The idea is to find a level of physical or mental activity you can manage without causing a major flare-up of your symptoms. The goal is to hover just below that trigger point, gently challenging your body's systems without overwhelming them.
For example, a physiotherapist might use a heart rate monitor to find a walking pace that boosts blood flow to your brain without triggering a headache. Over time, you gradually increase that threshold.
This concept is crucial because it turns recovery into an active, controlled process. It empowers you by teaching your body how to tolerate more, one step at a time.
Managing Energy and the Role of Medication
Your cognitive energy requires just as much management as your physical activity. This often involves breaking tasks into smaller chunks, scheduling rest breaks, and using strategies to reduce mental strain.
Medication can also play a supporting role, but it is rarely the entire solution. A doctor might prescribe something to help manage severe headaches, regulate a chaotic sleep cycle, or address underlying anxiety.
These medical interventions can provide the stability needed to fully engage with rehabilitation therapies. For readers wanting a structured overview of how these different treatments fit together, the entire process is explained in our comprehensive Concussion Guide.
Ultimately, a successful recovery is often about a coordinated, multi-pronged effort.
Taking the Next Step: From Understanding to Action
Understanding post-concussion syndrome is the first, most crucial step. Hopefully, this guide has helped frame PCS as a complex condition affecting multiple body systems, not a personal failing or an injury that is "taking too long" to heal.
When you can connect your symptoms to their underlying causes—such as fatigue with autonomic issues or dizziness with vestibular problems—that knowledge is empowering. It helps you have more productive conversations with healthcare providers and make more informed decisions. Moving from confusion to clarity is often the first feeling of control regained on the road to recovery.
Turning Knowledge into a Plan
Of course, an article can only provide a foundation. For those who are ready to build on this knowledge with a more structured approach, we have created a resource to help.
Understanding the 'why' behind your symptoms empowers you to take more effective action. It can transform recovery from a passive wait into an active, manageable process.
Our Concussion Guide was designed to be that next step. It takes the core ideas we've covered, like sub-symptom threshold activity and targeted rehabilitation, and lays them out in a practical, step-by-step framework.
Think of it as a roadmap to help you connect the dots between your diagnosis, treatment options, and daily self-management. It’s built to give you the confidence to work with your healthcare team and navigate your recovery.
Answering Your Questions About Post-Concussion Syndrome
Navigating the after-effects of a concussion can feel confusing. Here, we address some of the most common questions with straightforward, clinically-informed answers.
How Long Does Post-Concussion Syndrome Typically Last?
There is no single timeline, as each recovery is unique. While many people find their symptoms ease within three to six months, a smaller number may experience them for a year or longer.
Factors that can influence this include the nature of the injury, pre-existing health conditions like migraines or anxiety, and how quickly appropriate support is accessed. The focus should be on steady, gradual progress through active management rather than a specific end date.
Can You Get PCS Without Being Knocked Out?
Yes. It is a common misconception that loss of consciousness is required for a concussion or subsequent PCS. A concussion is caused by the brain's movement inside the skull, which disrupts function—this can happen with or without a blackout.
The defining characteristic of PCS is not what happened during the injury, but the persistence of symptoms beyond the expected recovery period.
Is It Safe to Exercise with Post-Concussion Syndrome?
Yes, but it must be the right kind of exercise. Carefully managed physical activity is a cornerstone of modern concussion care. The approach, called sub-symptom threshold exercise, involves staying active at a level that does not significantly trigger or worsen your symptoms.
A specialised physiotherapist can help you find your personal baseline and create a gradual plan with gentle activities like walking or stationary cycling. This controlled approach has been shown to help regulate blood flow in the brain and support recovery.
Is a Full Recovery from Post-Concussion Syndrome Possible?
For the majority of people, yes. The goal of treatment is to achieve a full functional recovery, where symptoms no longer dictate your life. With a targeted, multi-disciplinary approach, significant improvement and even a complete resolution of symptoms are achievable for most.
Some individuals may be left with mild sensitivities, but an active, evidence-based plan provides the best chance of returning to normal life. It is about active rehabilitation, not just passively waiting.
This article aims to provide clarity, but we understand that a blog post has its limits. For those wanting a structured path from understanding to action, The Patients Guide offers comprehensive resources that connect these concepts into a practical framework for recovery. Browse our library at https://www.thepatientsguide.co.uk.
Also in News
When Is the Best Time to Take Magnesium? A Guide to Timing Your Supplement
January 28, 2026 8 min read
Discover the best time to take magnesium for sleep, energy, or general health. Our guide explains how timing and type affect absorption and effectiveness.
Read More
Understanding Brain Fog Symptoms and Finding Clarity
January 27, 2026 11 min read
A calm, clear guide to understanding brain fog symptoms. Learn the common signs, potential causes, and practical next steps for managing mental fatigue.
Read More
Exercises for Neck Pain Relief: A Calm, Measured Approach
January 21, 2026 12 min read
A calm, structured guide to gentle exercises for neck pain relief. Learn safe, effective stretches and movements to manage discomfort and improve neck health.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
