Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
Understanding the Blood Count Test: A Clear Guide
February 06, 2026 14 min read
Receiving a request for a blood count test, or looking at a lab report filled with acronyms like RBC, WBC, and PLT, can be a confusing experience. It often feels like you are being asked to understand a language you haven't been taught.
If you have already searched for answers online, you may have found conflicting information or highly technical descriptions that create more questions than they answer. This is a common and understandable frustration.
A complete blood count (CBC) is one of the most routine tests in medicine, providing a broad snapshot of your overall health. It does this by counting and examining the different cells in your bloodstream.
This guide is designed to offer a clear, calm explanation of what a blood count test measures. The goal is not to provide medical advice, but to explain how healthcare professionals approach these results. We aim to help you feel more informed and better prepared for discussions with your doctor.
The Power of Data in Understanding Your Health
The real value of these tests is backed by enormous health initiatives. The UK Biobank, for example, has been collecting red blood cell count data from hundreds of thousands of people since 2012. This incredible pool of information helps clinicians across the country refine what's considered a 'normal' range.
These numbers tell a powerful story about preventative care. In the UK, NHS labs process an estimated 100 million of these tests every year, which helps catch conditions like anaemia early and often. It's a clear example of how your individual test contributes to a much bigger picture of public health.
Understanding your own results is an empowering first step. For readers wanting a structured overview beyond a single article, our library of patient guides offers more in-depth resources to support your understanding.
What a Full Blood Count Actually Measures
A Full Blood Count (FBC)—also known as a Complete Blood Count (CBC)—is a common blood test used in clinical settings. Think of it as a census of the cells in your bloodstream, giving your doctor a snapshot of your general health.
It’s a versatile tool, used for everything from routine health checks to diagnosing conditions or monitoring how a treatment is working.
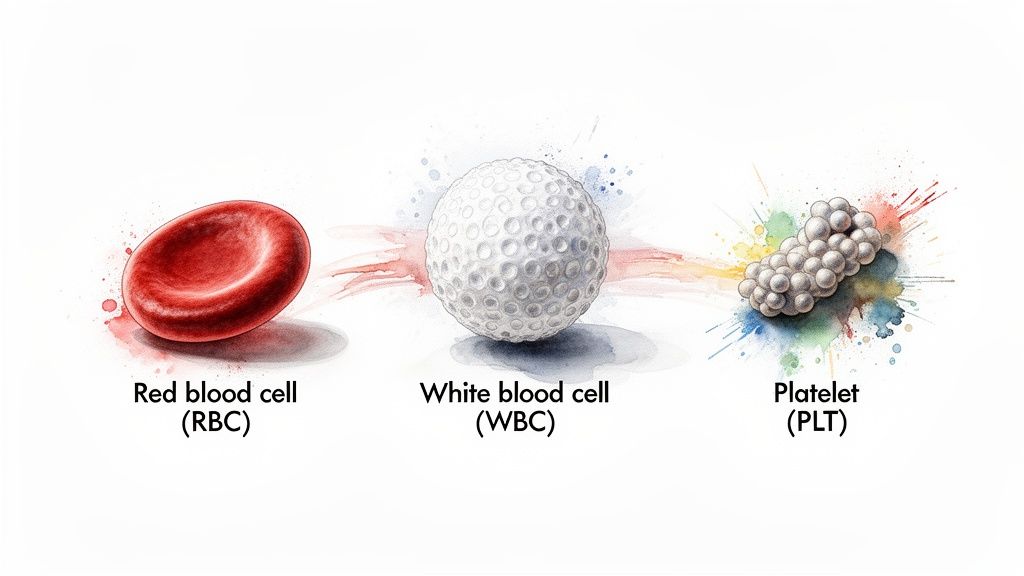
To understand what this test reveals, it can be helpful to think of your blood as a team. There are oxygen carriers (red blood cells), an immune defence force (white blood cells), and a repair crew (platelets). The FBC counts each of these, providing a report on how they are functioning.
This section will walk you through what each key component does, so you can start to see the picture your FBC paints. Let's look at the three main players measured in a Full Blood Count. Each has a distinct job, and the test measures not just their quantity, but often provides information about their size and shape, which can also be important.
Here’s a quick overview of what a clinician is looking at:
Key Components of a Full Blood Count
| Blood Component | Primary Function | What Clinicians Look For |
|---|---|---|
| Red Blood Cells (RBCs) | Transporting oxygen from the lungs to the rest of the body. | Count, size, and haemoglobin levels to check for conditions like anaemia. |
| White Blood Cells (WBCs) | Fighting infection and responding to inflammation. | The total count and a breakdown of different types to spot signs of infection or immune issues. |
| Platelets (PLT) | Helping the blood to clot and stop bleeding after an injury. | The platelet count to assess risks of bleeding or clotting problems. |
By analysing these components together, a healthcare professional can form a clearer idea of what may be happening inside your body.
The Oxygen Carriers: Red Blood Cells and Haemoglobin
The most numerous cells in your blood are your red blood cells (RBCs). Their main job is to carry oxygen from your lungs to every tissue and organ in your body.
They achieve this thanks to an iron-rich protein they contain called haemoglobin (Hgb). This is the molecule that binds to oxygen and also gives blood its red colour.
When assessing your red cells, the test measures several things:
- Red Blood Cell Count (RBC): The total number of red cells in your blood sample.
- Haemoglobin (Hgb): The total amount of this oxygen-carrying protein.
- Haematocrit (Hct): The percentage of your blood’s volume that is made up of red cells.
Your doctor looks at these figures together. If all three are low, for instance, it is a common indicator of anaemia. This condition means your body may not be getting the oxygen it needs to function optimally, which is why symptoms often include fatigue and weakness.
The Immune Defenders: White Blood Cells
Your white blood cells (WBCs) are a core part of your immune system. Though fewer in number than red cells, they are your body’s defence force, working to identify and address invaders like bacteria and viruses.
In clinical settings, an FBC often includes a 'differential'. This breaks down the total white cell count into the five main types of WBCs. Each type has a specific role, so observing which ones are high or low can give your clinician more specific clues about what your immune system is responding to.
This breakdown is very useful. For example, elevated levels of neutrophils often point towards a bacterial infection, while another type, lymphocytes, might be raised in response to a virus. Other types may signal an allergic reaction or inflammation.
The Clotting Agents: Platelets
Platelets are small cell fragments that act as first responders to injury. If a blood vessel is damaged, platelets are activated at the site.
They become sticky and clump together to form a temporary plug, which is the first step in the process of forming a blood clot to stop bleeding.
The FBC measures your platelet count (PLT):
- A low platelet count (thrombocytopenia) may be a concern because it could lead to easier bruising or prolonged bleeding.
- Conversely, a high platelet count (thrombocytosis) can sometimes increase the risk of forming unwanted blood clots.
These three core measurements—red cells, white cells, and platelets—are the foundation of a Full Blood Count. By examining their levels in relation to one another, your healthcare team can gain significant insight into how your body is functioning.
Understanding Normal Ranges and Why Context Is Key
When you receive a blood test report, your attention is often drawn to the column labelled ‘reference range’ or ‘normal range’. It is natural to feel concerned if any of your numbers fall outside of it.
Many people view an out-of-range number as an immediate red flag. However, these ranges are not rigid rules for health. They are better understood as statistical guidelines that show the typical values found in a large group of healthy people.
A result that is slightly high or low might not be clinically significant. In practice, healthcare professionals are often more interested in the overall pattern of your results and how they change over time.
So, What Is a "Normal Range" Anyway?
To establish these ranges, labs test a large, diverse group of people considered to be healthy. Statisticians then calculate the average range that 95% of these individuals fall into.
By definition, this means 5% of healthy people will have results outside the so-called "normal" range. Approximately 2.5% will be slightly below the cut-off, and 2.5% will be slightly above. An out-of-range result is often a statistical flag rather than a diagnosis.
A reference range is a guide, not a final verdict. Its main purpose is to help your clinician identify a result that might warrant a closer look, using your personal health history as the most important filter. This is why your doctor will interpret the numbers within the context of you.
Why Your Personal Story Matters Most
What is considered a ‘normal’ blood count can vary from one person to another. A value that is perfectly fine for you might be a point of interest for someone else. Clinicians are trained to consider several key factors:
- Age: Our blood cell counts naturally change as we get older. Newborns, for example, have different 'normal' ranges compared to adults.
- Sex: There are known differences in measurements like red blood cell and haemoglobin levels between men and women.
- Altitude: Living at a high altitude, where there is less oxygen, may cause your body to produce more red blood cells to compensate. This is a normal adaptation.
- Pregnancy: During pregnancy, the body undergoes significant changes that can naturally alter many blood count results.
Your wider health picture is also a crucial piece of the puzzle. A slightly low white blood cell count might warrant a closer look in someone with a fever, but could be insignificant in a healthy person with no symptoms. Clinicians connect these dots to look for patterns, not just isolated figures.
The Power of Your Own Baseline
In clinical thinking, comparing your current results to your own previous tests is often more valuable than comparing them to a generic population range. Over time, your blood tests establish a personal baseline that is unique to you.
A small shift from your typical baseline could be an early indication that something has changed, even if the new number is still technically within the standard normal range. This is one reason your doctor might suggest repeat tests—they are often looking for a trend.
This personalised approach can help identify potential issues sooner and avoid unnecessary concern over numbers that are simply normal for you. For instance, understanding the subtle signs of certain nutrient deficiencies can be key. To learn about a related test, you can find out more about the B12 blood test and its interpretation in our detailed article. This kind of knowledge helps build a more complete picture.
How Clinicians Interpret Common Patterns in Results
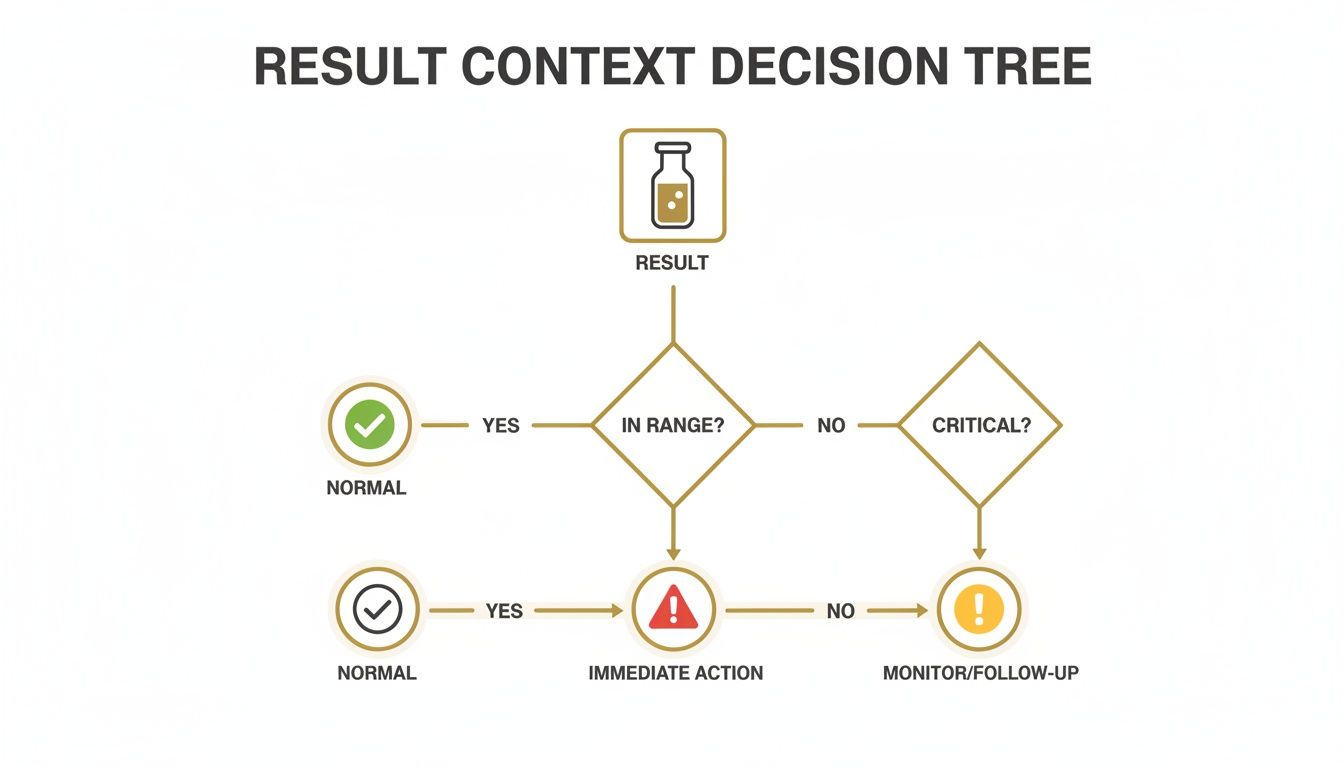
When a clinician reviews your blood count results, they look for patterns across the entire report rather than focusing on a single number. This process is like detective work, seeking clues that tell a story about what is happening in your body.
A single out-of-range value is one piece of data, but a pattern can be the beginning of a clinical assessment. It is the relationship between the different cell counts and their characteristics that often provides the most valuable insight, helping to narrow down possibilities.
The diagram above offers a simplified look at the thought process your clinician may follow when reviewing your results. The first step is always to place a result in context—deciding whether it needs monitoring, further tests, or no action at all.
The Story of Red Blood Cells: Uncovering Anaemia
One of the most common patterns clinicians look for is anaemia. This is a general term for having too few red blood cells or not enough haemoglobin, meaning the body may not be getting the oxygen it needs. This is often why people with anaemia feel tired and weak.
However, identifying anaemia is not the full story. The blood count provides additional details that help pinpoint the type of anaemia, which can point towards its likely cause.
- Low RBC, low haemoglobin, and small cells (low MCV): This combination often suggests iron deficiency anaemia. This may indicate the body does not have enough iron to build properly-sized, haemoglobin-rich red blood cells.
- Low RBC, low haemoglobin, and large cells (high MCV): In this case, the red blood cells are larger than normal. This pattern can be an indicator of a deficiency in vitamin B12 or folate, which are essential for healthy red blood cell production.
Distinguishing between these types is important because it informs the approach to treatment.
Clues From the White Blood Cell Family
Your white blood cell (WBC) count can act as a barometer for your immune system. A high total WBC count often means the body is fighting something. The differential—the breakdown of the five types of white cells—can provide more specific clues.
A common pattern is a high total WBC count driven by an increase in neutrophils. This is often a sign of a bacterial infection, like pneumonia or a urinary tract infection, as the body produces these 'first responder' cells to address the bacteria.
On the other hand, a viral infection can create a different picture. The total WBC count might be normal or even slightly low, but with a noticeable rise in lymphocytes. This tells the clinician the body has mounted a different type of immune response. For certain patient groups, understanding specific situations like managing a low white blood cell count during chemo is also vital.
Platelets and Their Links to Other Conditions
Platelet counts are rarely interpreted in isolation. A consistently low platelet count could be a primary blood issue, but it may also be an effect of another condition, such as an autoimmune disorder or liver disease.
A persistently high platelet count can sometimes be a marker for underlying inflammation or, in some cases, other conditions. In the UK, the full blood count has become an important tool in primary care for identifying potential issues early. Sometimes, non-specific symptoms like abdominal pain after eating can be part of a larger picture that a blood test helps to clarify.
An NIHR-funded study involving nearly 940,000 UK primary care patients showed that abnormalities like low haemoglobin or rising platelets, often found during tests for non-specific symptoms, can trigger specialist referrals. This shows how tracking trends over time can turn simple numbers into important clinical decisions. You can read the full research about these findings to learn more.
Your Test Day and Understanding Next Steps
Knowing what to expect on the day of your blood count test can help ease any nerves. For a standard Full Blood Count (FBC), you generally do not need to do any special preparation, such as fasting.
However, it is always best to follow the specific instructions from your healthcare provider, in case other tests are being run at the same time that do require it.
The Blood Draw Itself
The procedure for taking your blood, known as venepuncture, is usually quick. A phlebotomist or nurse will locate a suitable vein, typically on the inside of your elbow.
They will clean the area and then use a small needle to draw a sample of blood into one or more vials. You may feel a brief scratch, but the procedure is over quickly.
From there, your sample is sent to the laboratory. Automated analysers count and assess the different cell types in your blood. Results are often available within a few hours to a couple of days.
What Happens After You Get Your Results?
Receiving your results is not like getting a "pass" or "fail". How a doctor interprets your FBC report is about context—it depends on your overall health, your symptoms, and why the test was ordered.
Here are the most common next steps:
- No further action: If your numbers are within the normal range and there are no other concerns, the results will be added to your medical record.
- Monitoring: A result that is only slightly outside the normal range, especially if you feel well, might prompt your doctor to suggest monitoring. This often means repeating the test in a few weeks or months to see if it was a temporary fluctuation or if there is a developing trend.
- Further investigation: If the results show a more significant abnormality or point towards a specific issue, your doctor will likely order more targeted tests. This could involve more specialised blood work, an imaging scan, or a referral to a specialist.
The safety and reliability of blood tests today are based on rigorous standards. The Infected Blood Inquiry highlighted a tragic period between 1970 and 1991 where unscreened transfusions led to widespread infections. This history underscores the immense value of today’s highly screened blood supply in the UK, which is now 99.99% safe. A routine blood count test remains a vital tool for monitoring health. You can discover more insights about the statistics behind the inquiry on rss.org.uk.
Moving From Understanding to a Productive Conversation
Understanding your blood count results is an important first step. What follows is using that knowledge to have a productive conversation with your doctor or nurse.
The purpose of this guide is not to enable self-diagnosis. It is to empower you to be an active, informed partner in your healthcare. When you can speak the language of your results, you can ask more specific questions and better understand the reasoning behind your doctor's advice.
Your Role as an Informed Patient
Healthcare works best as a partnership. You bring your unique expertise—your symptoms, your lifestyle, and how you are feeling. Your clinician brings their medical training to interpret lab data within that personal context. This is where the most effective health decisions are made.
An effective healthcare discussion combines the clinical data from your blood count test with the real-world context that only you can provide.
With a basic understanding of the test, you can shift from being a passive recipient of information to an active participant in managing your health. This change in perspective is key to feeling more in control.
Asking the Right Questions
Arriving at your appointment with a few prepared questions can make a significant difference. It is not about challenging their expertise, but about ensuring you leave with clarity.
You could try asking questions like:
- "You mentioned my platelet count is on the low side of normal. Could you explain what that might mean in the context of my other results?"
- "Looking at my tests over the past year, are there any trends you are monitoring?"
- "Based on these results, what would you suggest as the next steps? What are we trying to rule out or confirm?"
Beyond the conversation, having access to reliable information is important. Providing patients with clear and trustworthy guides, like these top patient education resources, helps them build a stronger foundation of knowledge.
It’s important to remember that guides like this one have limits. They offer general knowledge, not personalised medical advice. The goal is to help you move past confusion and feel more confident in your health journey.
Frequently Asked Questions About Blood Count Tests
It is normal to have practical questions about your blood test. Here are some of the most common queries.
Can Diet or Stress Affect My Blood Count?
Yes, lifestyle factors can influence your blood results. Long-term diet plays a significant role. If you are not getting enough iron, vitamin B12, or folate, it can lead to types of anaemia that are visible in your red blood cell numbers.
Short-term factors can also have an effect. Significant dehydration can make your red blood cell count appear falsely high because the liquid portion of your blood is more concentrated. While a single stressful day is unlikely to cause major changes, chronic stress can contribute to inflammation, which may subtly alter your white blood cell count over time.
It is always a good idea to discuss your general diet and any major life stressors with your doctor when reviewing your results.
How Often Should I Get a Blood Count Test?
There is no single answer for this; it depends on your individual health. If you are generally well with no ongoing health issues, routine blood counts may not be necessary.
This changes if you are managing a chronic condition. For someone with kidney disease, an inflammatory condition, or a history of cancer, regular blood tests are often essential. They help your doctor track your condition and monitor treatment effectiveness. In these situations, your specialist will advise on the appropriate frequency.
Similarly, if you are experiencing persistent symptoms like fatigue, easy bruising, or recurrent infections, your GP will likely order a blood count as an initial step in their investigation.
What Is the Difference Between an FBC and Other Blood Tests?
A Full Blood Count (FBC) is a headcount of the cells in your blood—red cells, white cells, and platelets. Its purpose is to count and assess these physical components.
Other blood tests analyse the fluid component of your blood, known as plasma. They measure different substances to check how organs are functioning. For example:
- A Urea and Electrolytes (U&E) test assesses kidney function.
- A Liver Function Test (LFT) measures enzymes and proteins to check liver health.
- A lipid panel measures cholesterol to help assess cardiovascular risk.
In short, the FBC counts the cells, while chemistry tests analyse the chemicals dissolved in the blood's fluid. For more answers to common questions, you can also view our frequently asked questions section.
Why Are the Normal Ranges Different for My Child?
It is completely normal for a child’s blood count results to look very different from an adult’s. These "normal" ranges change continuously as a child grows.
Newborns, for example, have high levels of red blood cells and haemoglobin to adapt to breathing air. These numbers naturally decrease during their first year. The most common type of white blood cell also shifts from lymphocytes in young children to neutrophils in adults as their immune system matures.
Paediatric labs use specific, age-based reference ranges to interpret a child's FBC. This is a clear example of a key principle in medicine: context is everything, and what is ‘normal’ depends entirely on the individual.
At The Patients Guide, we create structured, in-depth resources to help you understand your health with clarity. For those who want to move beyond articles and gain a more organised understanding of specific conditions, we invite you to explore our library of guides at https://www.thepatientsguide.co.uk.
Also in News

A Calm Guide to Treating Whiplash at Home
February 10, 2026 10 min read
Feeling overwhelmed by neck pain after an injury? This is a calm, clear guide to treating whiplash at home, focusing on safe pain relief and recovery.
Read More
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
