Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Modern healthcare is fragmented. Understanding your condition helps connect the dots.
Library
FEATURED
HEALTH HIGHLIGHT
FEATURED
Understand your triggers, find relief that works, and stop migraines from ruling your life.
HEALTH HIGHLIGHT
Learn how to protect your bones, reduce risk of fractures, and take charge of your bone health at any age.
MINI GUIDES
Get quick answers, learn proven tips, and take action with our bite-size mini guides.
A Patient's Guide to the B12 Blood Test
February 05, 2026 12 min read

If you're looking into a B12 blood test, you are likely trying to make sense of persistent symptoms like fatigue, brain fog, or strange neurological sensations. Searching for answers online often leads to conflicting advice, leaving you feeling more confused than when you started.
One site might suggest a simple dietary change, while another discusses complex autoimmune conditions. This can feel overwhelming, especially when you just want a clear explanation for what you are experiencing.
This guide is designed to provide a calm, grounded overview of the B12 blood test from a clinical perspective. We will explain why this test is used, what the results mean in a real-world context, and what you can expect afterwards. The goal is to reduce uncertainty, not to offer quick fixes.

Why This Test Is an Important First Step
Understanding the purpose of a B12 blood test helps you have a more productive conversation with your doctor. It is more than just a number; it’s a key diagnostic tool that can link your symptoms to a potential, and often very treatable, underlying cause.
Vitamin B12 is essential for several fundamental processes in the body:
- Nerve Health: It helps maintain the myelin sheath, a protective layer around your nerves that is critical for proper signalling.
- Red Blood Cell Formation: The body cannot produce healthy red blood cells without it. These cells are responsible for carrying oxygen to every part of your body.
- DNA Synthesis: It plays a vital role in creating and repairing your body's genetic material.
When B12 levels become too low, these core functions can falter, leading to the wide range of symptoms that commonly prompt a healthcare professional to order this test.
In clinical settings, a B12 test isn't just a measure of a vitamin. It provides a valuable snapshot of your nervous system's health and your body's ability to produce energy.
This guide will walk you through the clinical reasoning behind the test, helping to clarify the journey from symptom to diagnosis. To understand the broader role these nutrients play, you can explore our resources on B Vitamins. Building this foundational knowledge can help you partner more effectively with your healthcare provider.
Why Clinicians Recommend a B12 Test
When a GP suggests a B12 blood test, it is typically a calculated step based on specific clues from your symptoms, medical history, or lifestyle. It is a targeted investigation aimed at uncovering a potential—and treatable—reason for how you are feeling.
Healthcare professionals are trained to recognize patterns. When a patient describes a certain combination of neurological or energy-related symptoms, B12 deficiency is a common possibility they consider.
Common Patterns: Nerve and Blood-Related Symptoms
Vitamin B12 is crucial for maintaining a healthy nervous system and for producing red blood cells. When levels are low, these two systems are often the first to show signs of distress.
A doctor may consider a B12 test if you report:
- Neurological Symptoms: This can include persistent pins and needles (paraesthesia), numbness, unsteadiness, memory issues, or poor coordination. These symptoms may arise because low B12 can affect the protective myelin sheath around your nerves.
- Signs of Anaemia: Constant fatigue, pale skin, shortness of breath, or a sore, red tongue are common indicators. A full blood count showing unusually large red blood cells (macrocytic anaemia) is a significant finding that often leads to a B12 test.
While these symptoms can be caused by other conditions, they are strong enough indicators to warrant investigation.
Key Risk Factors That Prompt Testing
Sometimes, a test is recommended even before significant symptoms appear. This is because certain health conditions, diets, or age can increase the risk of developing a deficiency.
A GP is likely to suggest a test if you fall into one of these groups:
- Age: Individuals over 60 are at higher risk. Stomach acid production tends to decrease with age, and this acid is needed to release B12 from food.
- Diet: A strict vegan or vegetarian diet is a well-known risk factor if not managed with supplementation. B12 is primarily found in animal products.
- Gastrointestinal Conditions: Issues affecting the stomach or small intestine—such as Crohn's disease, coeliac disease, or atrophic gastritis—can impair the body's ability to absorb B12.
- Certain Medications: Long-term use of some common drugs can interfere with B12 absorption. Metformin (for diabetes) and proton pump inhibitors (for acid reflux) are common examples.
In practice, the decision to test is often based on a combination of listening to a patient's experience and identifying these established risk factors. The goal is to detect a deficiency early to prevent more serious or long-term health issues.
Vitamin B12 deficiency is more common than many people realise. In the UK, it affects around 6% of people under 60 and rises to 20% in those over 60. Given its prevalence, the B12 blood test is a vital diagnostic tool, especially as pernicious anaemia is the leading cause of severe deficiency in the country. You can read the official guidelines for B12 testing on nice.org.uk.
Understanding this clinical reasoning can make the process feel less arbitrary. If you want to explore dietary influences further, you can find more information about optimising your diet and nutrient intake in our nutrition section.
How to Interpret B12 Test Results
Receiving a lab report can be confusing. The key thing to remember about your B12 blood test results is that the numbers are only one part of the clinical picture. Their true meaning is revealed when considered alongside your symptoms, health history, and the specific reference ranges used by the lab.
This section aims to help you understand what 'deficient', 'borderline', and 'normal' mean in a UK clinical context, so you can have a clearer conversation with your doctor.
Total B12 vs. Active B12: An Important Distinction
The standard B12 blood test measures Total B12. This value represents all the vitamin B12 in your bloodstream. However, not all of this B12 is available for your body's cells to use.
A useful analogy is a delivery truck full of packages:
- Total B12 is like all the packages on the truck. It tells you the overall quantity.
- Active B12 (holotranscobalamin) is like the packages that are correctly addressed and can be delivered and used.
The Total B12 test is commonly used because it is reliable and cost-effective. However, it's possible for someone to have a normal Total B12 level while having low Active B12, which can still lead to deficiency symptoms. This illustrates why a single test result doesn't always provide the complete picture.
Understanding Your B12 Test Results (UK Adult Ranges)
Your lab report will show your B12 level next to a 'reference range'. To understand your test results, it helps to know what is the normal range for vitamin B12. While ranges can vary slightly between labs, their interpretation in the UK generally follows a common pattern.
The table below outlines typical serum B12 levels and how they are commonly interpreted. These are general guidelines; your GP will interpret them based on your individual circumstances.
| B12 Level (ng/L) | Common Interpretation | Potential Next Steps |
|---|---|---|
| Below 180 | Deficient. Deficiency is highly likely, and treatment is usually recommended to prevent or address symptoms. | Your GP will likely suggest B12 injections to restore your levels. Further tests to find the cause may follow. |
| 180 - 350 | Borderline or indeterminate. This is a grey area where deficiency is possible, particularly if you have symptoms. | Your GP will consider your symptoms and risk factors. They may suggest a follow-up test (like Active B12) or a trial of B12 treatment to see if symptoms improve. |
| Above 350 | Normal. A B12 deficiency is considered unlikely. | If symptoms persist, your GP will likely investigate other potential causes. Monitoring may be advised if you have ongoing risk factors. |
The most crucial point is that clinicians interpret the number in the context of your personal experience to decide on the appropriate course of action.
Why Your Symptoms Are a Critical Part of the Picture
The flowchart below illustrates how clinical decisions are often made. The process starts with you—either with the symptoms you're experiencing or known risk factors.
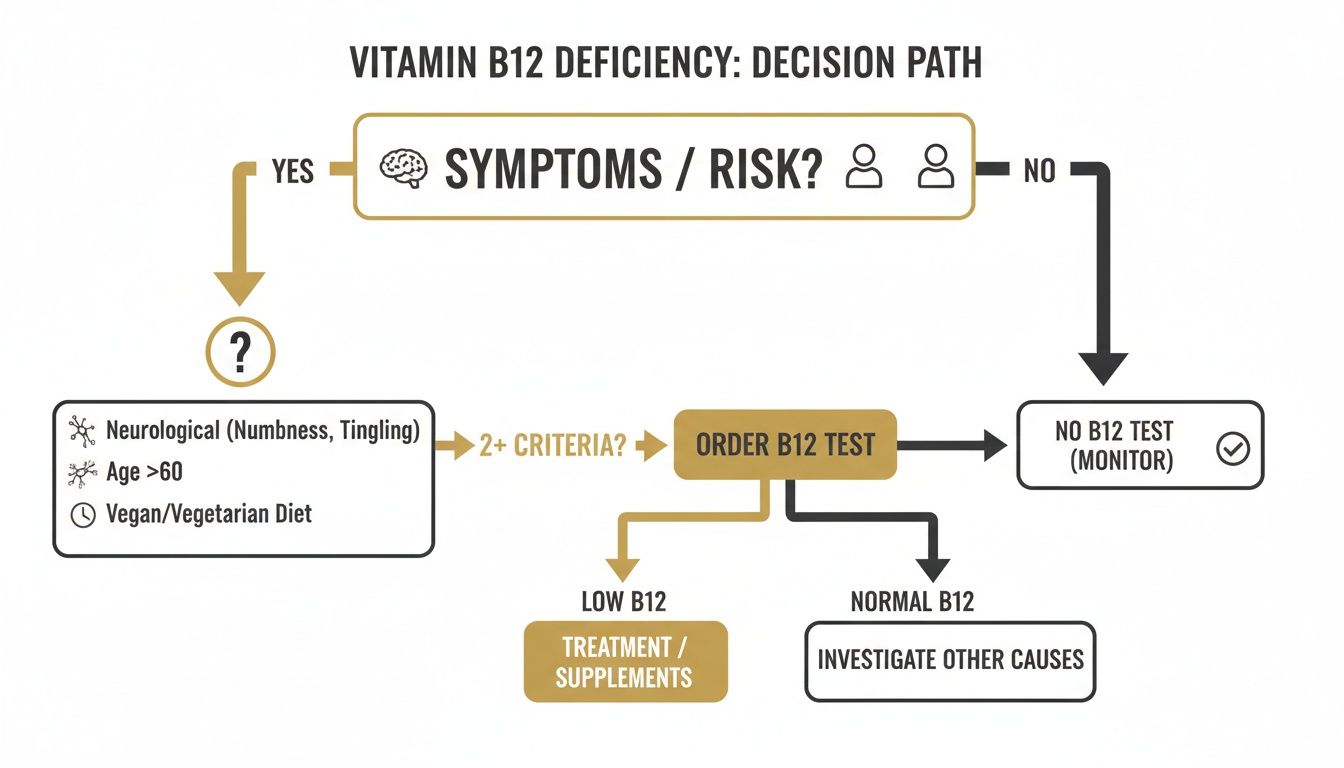
This shows why two people with the same 'borderline' result might receive different advice. Someone with neurological symptoms may be offered treatment, while someone with no symptoms may be advised to simply monitor their levels.
This is a patient-centred approach. Your reported symptoms and clinical signs are considered just as important as the number on the lab report.
This ensures that treatment decisions are guided by your health needs, not just by a lab value alone.
Navigating The Different Types Of B12 Tests
When a B12 deficiency is suspected, the initial test is often just the first step in the investigation. Obtaining a clear diagnosis is not always straightforward. A clinician will consider all the evidence—symptoms, medical history, and results from one or more B12 tests—to determine the most likely cause.
The Standard Serum Total B12 Test
The most common initial test used by the NHS is the serum total B12 test. It measures the total amount of vitamin B12 in the blood, providing a solid baseline reading.
The limitation of this test is that it cannot distinguish between the 'active' form of B12 that your body can use and the 'inactive' form that is bound to other proteins. It's possible to have a "normal" result but still experience a functional deficiency at a cellular level.
The Active B12 Test (Holotranscobalamin)
If the initial test result is borderline or doesn't align with your symptoms, a more specific test may be considered. This is where the active B12 test can be useful.
Also known as the holotranscobalamin test, it measures only the B12 that is attached to its transport protein, transcobalamin. This is the form that can be delivered to and used by your body's cells. This test can provide a clearer insight into whether you have enough usable B12.
For a closer look at what this assessment involves, you can find detailed information on tests like the Vitamin B12 Active test.
Building a More Complete Picture with Further Tests
A single number from one B12 blood test rarely tells the whole story. To investigate further, a doctor might order other tests to gather more clues and identify the root cause.
These supporting tests help to fill in the details:
- Folate Levels: B12 and folate work together, and a folate deficiency can cause similar symptoms. It can also mask a B12 deficiency in some blood tests, so checking both is standard practice.
- Intrinsic Factor Antibodies (IFAB): This test is important if pernicious anaemia is suspected. Intrinsic factor is a protein needed to absorb B12 from food. If your immune system produces antibodies against it, this strongly suggests an autoimmune cause.
- Methylmalonic Acid (MMA): This is a "functional" marker. When cells don't have enough B12, levels of MMA can build up in the blood. An elevated MMA level is a strong indicator of a B12 deficiency at the cellular level, even if the serum B12 result seems normal.
In clinical practice, these results are used like pieces of a puzzle. A borderline total B12, combined with neurological symptoms and a high MMA level, presents a much clearer picture than the B12 result alone.
This layered approach helps explain why reaching a diagnosis can sometimes take time. It is a methodical process designed to build a complete biological picture of your health.
What to Expect After a Low B12 Result
Receiving a low result from your B12 blood test can feel concerning, but it is often a positive step. It means you are moving from uncertainty toward a clear treatment path. Well-established clinical guidelines exist for restoring B12 levels safely and effectively.
In the UK, a confirmed deficiency is not typically treated with dietary advice alone, especially if an absorption issue is the cause. The standard approach is more direct.

The Standard Treatment: B12 Injections
For most people diagnosed with a B12 deficiency, particularly if neurological symptoms are present, the standard treatment is a course of B12 injections. The form of B12 most commonly used by the NHS is hydroxocobalamin.
Injections are used because they bypass the digestive system entirely, delivering the vitamin directly into the muscle for absorption into the bloodstream. This ensures the B12 reaches your system, which is critical if the underlying cause is an absorption problem like pernicious anaemia.
The Loading and Maintenance Dose Schedule
Treatment typically begins with an intensive phase to quickly replenish the body's B12 stores. This is often referred to as a 'loading' dose.
A common schedule includes:
- Intensive Phase: An injection every other day for approximately two weeks to rapidly increase B12 levels.
- Maintenance Phase: After the initial course, the frequency is reduced. A maintenance injection is then typically given every 2 to 3 months, often for life, if the cause of the deficiency is permanent.
This structured plan aims to provide both immediate support and long-term stability. Your GP will tailor the schedule based on your specific needs and response to treatment. While injections are the standard medical approach for absorption issues, you can learn about other forms, such as our vitamin B12 methylcobalamin supplement.
What If My Results Are Borderline?
If your B12 test result is in the 'borderline' range, the next steps are less defined. In this situation, how you feel becomes a very important factor.
Your GP may suggest a 'therapeutic trial' of B12 injections. This involves giving the standard loading doses to see if your symptoms improve.
A therapeutic trial serves as a practical diagnostic tool. If your symptoms get better with treatment, it provides strong evidence that a functional deficiency was the problem, regardless of the initial lab number.
This patient-centred approach ensures that treatment is guided by your real-world experience, acknowledging that blood tests have limitations and the ultimate goal is to resolve symptoms.
Growing awareness is reflected in NHS prescribing data. In England, prescriptions for vitamin B12 rose from 57 million in 2015 to over 63 million by 2024. This trend, noted in a detailed analysis of UK B12 testing, underscores the importance of this blood test in identifying a common condition.
Finding Your Path Forward With Clarity
A B12 blood test is an important diagnostic tool, but the result is not the full story. True clarity comes from understanding that number in the context of you—your symptoms, your health history, and your lifestyle. A single figure on a lab report is just one piece of a larger puzzle.
This article aimed to help you feel more informed about why a B12 test is ordered, what the results may mean, and what the potential next steps are. It is about connecting how you feel with what the data shows, leading to a diagnosis that makes sense.
Beyond The Blog Post
An article like this can provide a solid foundation and help you feel more prepared for discussions with a clinician. However, individual health situations are complex and rarely fit neatly into a single explanation.
While blogs are useful for explaining specific topics, they often struggle to connect all the dots. They may not show how your B12 status relates to other nutrient levels, your diet, or your overall health strategy in a coherent, long-term way.
Recognising the need for a more organised approach is an important step. It marks a shift from collecting isolated facts to building a connected understanding of your health.
For readers who are ready for a deeper, more structured overview, we have created resources to help.
A Structured Next Step
We created The Patient's Guide for people who want to move beyond individual articles and build a comprehensive understanding of their health. Our guides are designed to connect the concepts we’ve discussed here into a practical, logical framework.
This is not a replacement for medical advice. It is a tool to empower you as an informed partner in your own healthcare. It represents a logical next step for those seeking a sustainable path forward.
Frequently Asked Questions
It is normal to have questions when navigating a health issue. Here are straightforward answers to common queries about B12 testing and treatment.
Will I Need to Fast For My B12 Blood Test?
Generally, no. Fasting is not usually required for a B12 blood test. Unlike cholesterol or glucose tests, your recent food intake does not significantly affect your B12 levels.
However, it is always wise to confirm with the clinic or your GP's office. Sometimes, other tests that do require fasting are run from the same blood sample. A quick check can prevent a wasted journey.
Should I Stop B12 Supplements Before the Test?
Yes, this is very important for an accurate result.
Taking supplements containing vitamin B12, including multivitamins, can artificially raise the B12 levels in your blood. This can mask an underlying deficiency, leading to a falsely "normal" reading that doesn't reflect your body's true status.
Most clinicians recommend stopping all B12 supplements for at least one to two weeks before your blood test. Always inform the healthcare professional about any supplements you have recently taken.
How Long Does It Take For B12 Injections to Work?
Each person's response is different. Many people report an improvement in energy levels within the first few days or weeks of starting the initial 'loading dose' injections.
Neurological symptoms, such as pins and needles or cognitive fog, often take longer to improve. It may take several months of consistent treatment to see significant changes. In some cases, the primary goal is to prevent these symptoms from worsening. Patience and adherence to the prescribed injection schedule are key.
Can I Have B12 Deficiency With a Normal Blood Test?
Yes, it is possible to have the classic symptoms of B12 deficiency even when a standard blood test shows a normal result. This is sometimes referred to as a ‘functional’ or ‘cellular’ deficiency.
This can occur when there appears to be enough B12 in the bloodstream, but the body has difficulty transporting it into the cells where it is needed.
If your symptoms strongly suggest a deficiency despite a normal test, your clinician may recommend further tests, like an active B12 or MMA test, or suggest a therapeutic trial of B12 injections to see if your symptoms respond.
You can find more answers to your health queries by exploring our full list of Frequently Asked Questions.
At The Patients Guide, we create structured, in-depth resources to help you connect symptoms, tests, and treatments into a clear picture. If you're looking for a step-by-step approach that goes beyond individual articles, explore our library.
Also in News

A Calm Guide to Treating Whiplash at Home
February 10, 2026 10 min read
Feeling overwhelmed by neck pain after an injury? This is a calm, clear guide to treating whiplash at home, focusing on safe pain relief and recovery.
Read More
Dizziness Before Periods: Understanding the Causes and Patterns
February 09, 2026 9 min read
Discover the root causes of dizziness before periods and learn practical, gentle strategies to ease symptoms and feel better fast.
Read More
Understanding Epithelial Cells in Urine Test Results
February 08, 2026 10 min read
Confused about epithelial cells in urine on your test results? Our guide explains what they mean, from contamination to kidney health, in clear, simple terms.
Read More
Subscribe
Sign up to get the latest on updates, new releases and more …
